Contents
Introduction
Pathology
Clinical Features
Investigations
Treatment
Introduction
Pneumonia is an infection of the lung that is characterised by the presence of exudate in the alveoli. It is a common condition and has an incidence of approximately 300 per 100,000 per year. Although any age can be affected the young and the elderly are at most risk. The male : female ratio is generally equal.
The risk factors include the following.
- Extremes of age
- Immunosuppression
- COPD
- Brochiectasis
- Tumour or other cause of bronchial obstruction
- Cardiac failure
- Ciliary dysfunction (including smokers)
Pathology
Pneumonia is divided into two types, lobar pneumonia and bronchopneumonia. Pneumonia is usually acquired by inhalation but the haematogenous and aspiration routes may also occur.
Lobar pneumonia tends to affect previously fit and well people who have no predisposing factors to pneumonia. The causative organism is usually streptococcus pneumoniae. Lobar pneumonia is confined to one lobe and is sharply demarcated from the adjacent lobes of the lung.
Lobar pneumonia is considered to have four stages. The basic pathological process is that of
acute inflammation.
The first stage occupies the first 1-2 days and is called acute congestion. The acute inflammatory system is activated in response to infection of the airspaces by bacteria. Vasodilatation and hyperaemia occur. Increased capilliary permeability causes fluid to leak into the alveoli. This fluid contains erythrocytes, neutrophils and fibrin. Bacteria are also numerous. The affected lobe is red (hyperaemia), heavier than usual and frothy when squeezed (oedema due to increased capillary permeability).
Acute congestion is followed by red hepatisation which occupies days 2 to 4. The lobe is red, heavy and airless and allegedly resembles liver. The affected lobe is dry. The neutrophils have been kicking bacterial butt and the number of bacteria in the alveoli will have fallen. Both neutrophils and erythrocytes are numerous. The fibrin fibres are cross-linked to form a fine network.
The pleural surface may bear small grey-white tags of fibrin.
The filling of the airspaces by the liquid / semi-solid inflammatory exudate (pus) is known as consolidation.
Grey hepatisation is seen in days 4 to 8. The lobe is now grey, heavy, airless and dry. Having defeated the enemy the neutrophils are largely dead or disintegrating; the erythrocytes are also no more. The fibrin network is now dense.
The fibrinous pleurisy is now more established.
Resolution is the fourth stage and begins around day eight. The infection has been defeated. Macrophages move into the lobe and begin the clear up operation of removing the mess; fibrinolytic enzymes help to render the debris more easily phagocytosable.
Resolution requires one to three weeks. Once it is completed it is often impossible to tell that that lobe was ever inflamed. More marked infections may result in fibrous adhesions between the two layers of the pleura.

|
A right lung which shows upper lobe lobar pneumonia
Courtesy of the pathology museum, St George's Hospital
|
Bronchopneumonia affects people who have one or more predisposing factors. Rather than being restricted to one lobe the infection is more disseminated and is centred on the bronchioles rather than the alveoli (which become involved by extension of the infection from the bronchioles). Consolidation develops and the microscopic features are similar to lobar pneumonia. Squeezing the lung may cause pus to be expressed from the airways.
Full resolution is less likely in bronchopneumonia. The infection and inflammation can damage the walls of the bronchioles and in severe cases
bronchiectasis may result.

|
A left lung which exhibits bronchopneumonia in its lower portion
Courtesy of the pathology museum, St George's Hospital
|
Microbiology
The commonest causative organism of pneumonia is streptococcus pneumoniae. The second commonest is probably mycoplasma pneumoniae (which may tend more to a tracheobronchitis). Other organisms include klebsiella pneumoniae, legionella pneumophilia (Legionnaire's disease), staphylococcus aureus, coxiella burnetti (Q fever), chlamydia psittaci (psittacosis), pseudomonas aeruginosa, mycobacterium tuberculosis and pneumocystis carinii (seen in AIDS). Various virus are also capable of having a bash at pneumonia.
Haemophilus influenzae is a common organism in patients who have
chronic obstructive pulmonary disease. It is often called "H 'flu" in speech.
An atypical pneumonia is one which is caused by organisms such as mycoplasma pneumonia. Atypical pneumonias tend to show a lack of correlation between the clinical features and the findings on chest X-ray, as well as having presentations which do not fit neatly into the model exemplified by streoptococcus pneumoniae and haemophilus influenzae, often because various extrapulmonary manifestations are encountered.
Aspiration pneumonia is a term applied to a pneumonia which is the result of aspirating gastric contents into the lungs. It usually occurs in people who have uncoordinated swallowing (for example, after a stroke) or who are unconscious (other than sleep). The organisms are typically assorted Gram negative rods. If the patient dies the defining feature at post mortem is the presence of food in the distal airways.
Clinical Features
Pneumonia presents with dyspnoea and a cough that is productive of purulent yellow to green sputum. A small degree of haemoptysis can be admixed. The patient usually has a fever. Involvement of the pleura by the inflammation will yield pleuritic chest pain in which the patient experiences sharp chest pain over the affected part of the lung when they breathe in or cough. The pain can cause the patient to breathe more shallowly.
On examination the patient may be tachypnoeic; cyanosis is rare. The trachea is central. Expansion is reduced in the affected part (or parts of the lungs) because the presence of consolidated gunge in the airways means that air cannot enter. The percussion note is dull. The breath sounds have shifted from vesicular to bronchial and may feature crackles. A pleural rub may also be heard when the two layers of inflamed pleura rub against each other. Vocal resonance is increased.
Pneumonia may be complicated by a pleural effusion, lung abscess, respiratory failure, septicaemia and
SIADH.
Investigations
Although the diagnosis of pneumonia is frequently straightforwards there are various investigations that should be performed.
Sputum should be sent for culture, microscopy and sensitivity in order to determine that appropriate antibiotic therapy is being used. Sputum samples are sometimes supplemented by blood cultures.
A full blood count is necessary to determine if their is leucopenia or severe leucocytosis (both denote a severe pneumonia). The haemoglobin level is also useful because co-existent anaemia can exacerbate the dyspnoea and the impairment of lung function.
The urea and electrolytes are required because renal impairment is a criterion for admission. The U+E also address the rare possibiliity of SIADH.
A low albumin signifies a patient who is at a higher risk and therefore should be admitted. The determination of the albumin level requires liver function tests to be performed.
A chest X-ray is central to the confirmation of the diagnosis.
|
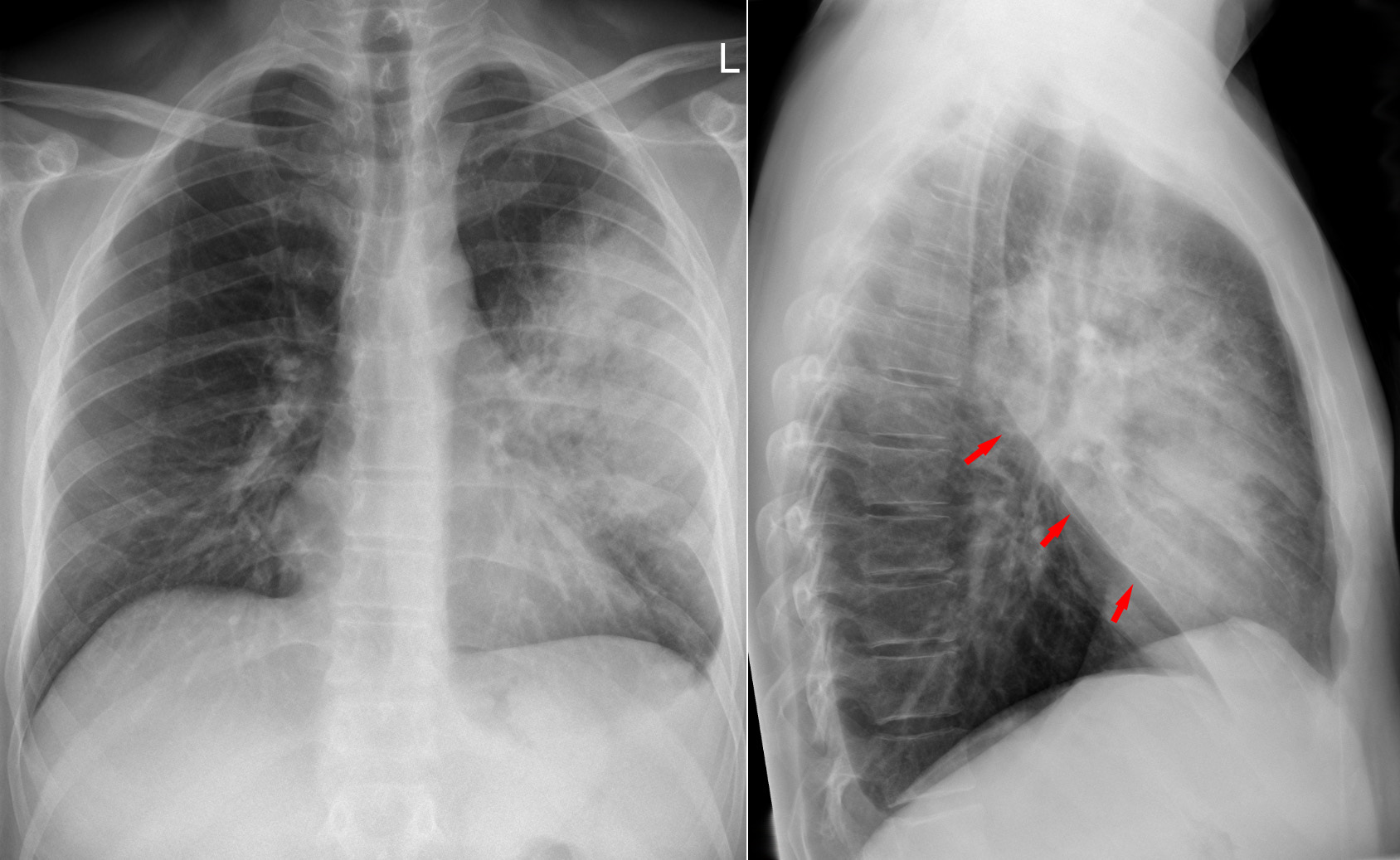
A standard chest X-ray and a lateral chest X-ray of left upper lobe pneumonia. The red arrows indicate the oblique fissure.
Courtesy of Wikipedia
|
|
|
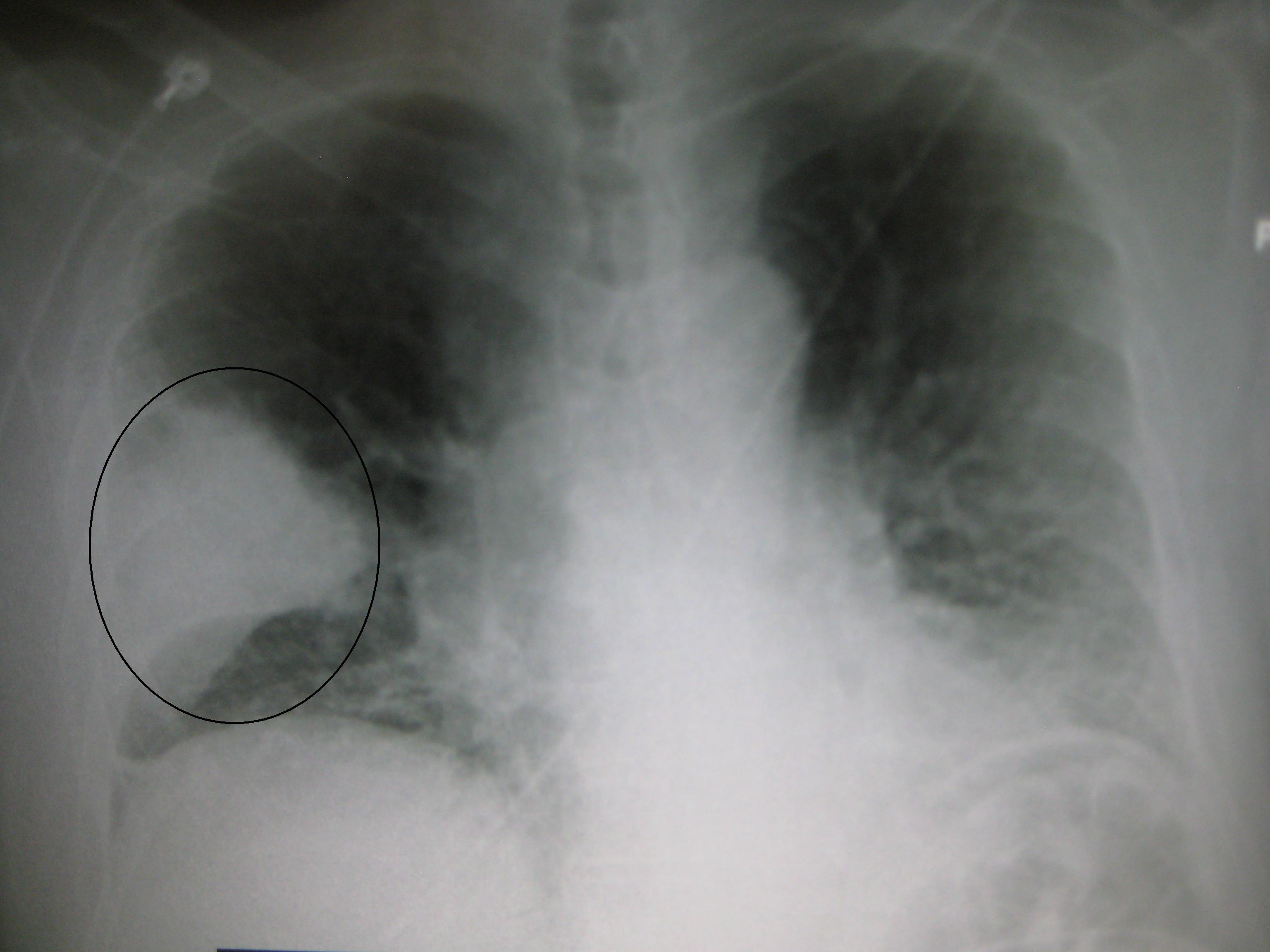
A chest X-ray of a right middle lobe pneumonia
Courtesy of Wikipedia
|
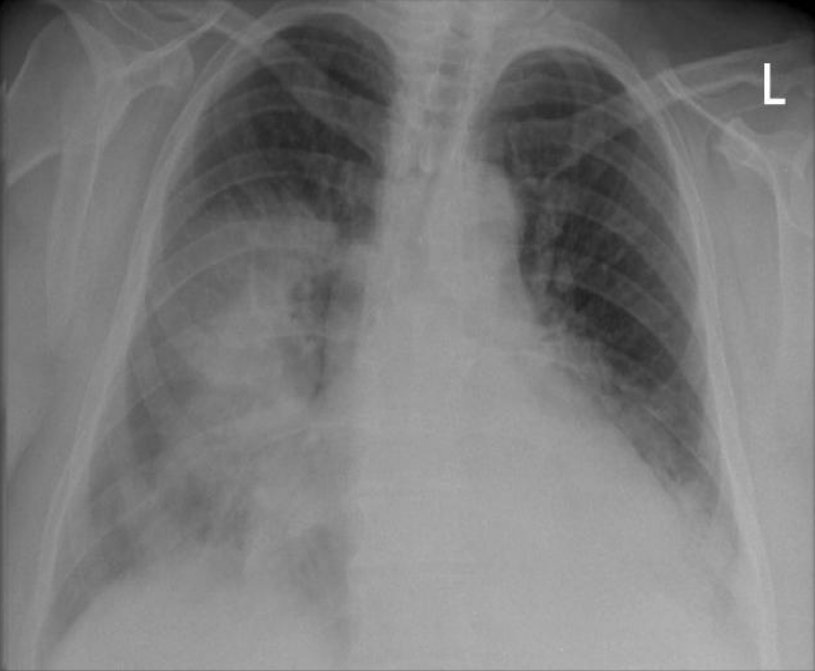
A chest X-ray of right middle and right lower lobe pneumonia
Courtesy of Wikipedia
|
Treatment
Treatment is with antibiotics. A popular choice if the causative agent is not known for certain is a beta-lactam (such as amoxycillin) combinted withh a macrolide (such as erythromycin). This will cover most of the likely organisms that can be acquired in the community and also addresses atypical organisms such as mycoplasma. If there are reasons to suspect different infectious organisms (for example aspiration pneumonia, bronchiectasis) or if the microbiology results reveal an unusual organism a different choice of antibiotics will be employed.
Patients often benefit from analgesia for the pleuritic pain. Oxygen may be helpful.
The prognosis in lobar pneumonia is excellent. Bronchopneumonia is also eminently treatable but the outcome will be influenced by the patient's pre-existing illnesses.
Patients who have had pneumonia should have a chest X-ray after the episode has resolved to check that there is no underlying tumour.