Contents
Introduction
Uterine leiomyomas are popularly known as fibroids and are benign smooth muscle tumours of the myometrium. They are common although are frequently asymptomatic; approximately 25% of women have one or more leiomyomas. Fibroids are more common in black women. The cause of uterine leiomyomas is unknown, although the tumours require oestrogen and progesterone; obsesity and hypertension are risk factors.
Pathology
Uterine leiomyomas can be single, several or multiple in any given uterus and can have a wide range of sizes. However, they all possess a very similar, characteristic macroscopic appearance of circumscribed, well-defined grey-white ovoid masses that have a whorled cut surface. It is not unusual for a leiomyoma to seem to shell out from the adjacent myometrium.
Leiomyomas can be found in three positions within the myometrium: submucosal, intramural and subserosal. Submucosal fibroids are most likely to distort the shape of the uterine cavity. Large and/or multiple fibroids can increase the surface area of the endometrium and produce
menorrhagia. If a submucosal fibroid is particularly pedunculated and hangs in the endometrial cavity the uterus may attempt to expel it during menstruation and this is an unusual mechanism by which fibroids can cause
dysmenorrhoea.
Subserosal fibroids are sometimes pedunculated. On rare occasions a very pedunculated subserosal fibroid can attach to another organ, acquire a blood supply and lose its uterine pedicle; such a leiomyoma is known as a parasitic leiomyoma.
|
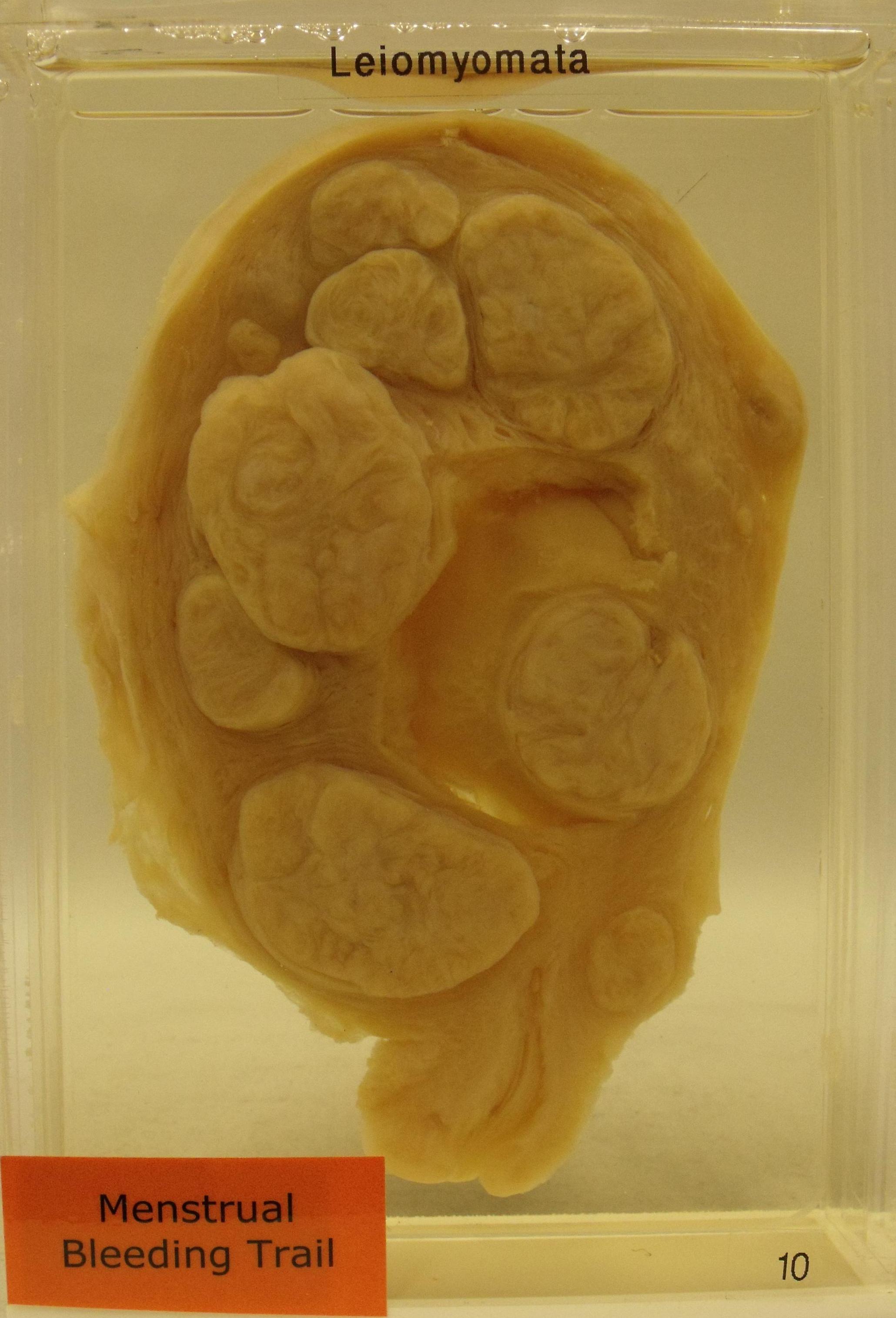
This uterus contains nine fibroids. The protrusion of the fibroid above the cut surface of the myometrium is characteristic in a fixed specimen.
Image courtesy of Dr Carol Shiels
|
Microscopically leiomyomas are composed of fascicles of uniform smooth muscle cells. The cellularity of the leiomyoma is usually greater than that of the adjacent myometrium. Mitotic activity is usually scarce, as are mitoses. Hyaline change, myxoid change or calcification can be encountered in older leiomyomas. Red degeneration is a complication that occurs during pregnancy and is due to thrombosis of the blood vessels that supply the leiomyoma.
Several microscopic subtypes of leiomyoma have been described. Mitotically active leiomyomas show neither necrosis nor cellular atypia but have an increased number of mitoses (at least 5 per 10 high power fields). A cellular leiomyoma possesses a markedly increased cellularity. The epithelioid leiomyoma is composed of epithelioid rather than spindle-shaped smooth muscle cells. The symplastic leiomyoma manifests cytological atypia but no necrosis or elevated mitotic activity.
Intravenous leiomyomatosis is a very rare condition in which nodules of smooth muscle cells grow within veins around the uterus. Even more rarely these masses can extend into the inferior vena cava andthe right side of the heart.
Possibly one of the most peculiar terms in histopathology is that of benign metastasising leiomyoma. Patients who have this rare condition demonstrate leiomyomatous masses in the lungs, lymph nodes and abdomen that are believed to be of uterine origin. These masses are benign yet somehow are deemed to have metastasised.
Cut Up
If surgery is performed to treat fibroids the specimen may either be a myomectomy, subtotal hysterectomy, total hysterectomy or total hysterectomy with bilateral salpingo-oophorectomy. These specimens are cut up as for the
general approach to a hysterectomy and the standard blocks are taken in addition to those relating to the fibroids.
The macroscopic inspection of the fibroids is of crucical importance in both hysterectomies and myomectomies. If all the fibroids have the typical appearance and do not show abnormal regions then only three blocks of the fibroids are necessary. This applies whether there is one fibroid or twenty or more. Any abnormal looking mass should be sampled more thoroughly: the concern for these atypical lesions is that there are a leiomyosarcoma or other sinister neoplasm.
The macroscopic evaluation of a fibroid requires that it is sliced thoroughly. Bisecting a 100mm diameter fibroid is not sufficient; it must be divided into multiple slices as almost any other solid tumour would be. The consequence of this diligence is the ability to take a small number of blocks. For a hysterectomy specimen this may require that the uterus is divided into several or more parallel parasagittal slices.
In essence, much of the diagnosis of a uterine leiomyoma occurs at the macroscopic level; the blocks serve to confirm this macroscopic impression. The pathologist is given credit for an ability to recognise fibroids macroscopically and to identify when something is amiss macroscopically; the blocks could be considered to be akin to quality control of this macroscopic diagnosis.
Clinical Features
The majority of fibroids are asymptomatic. Those that do cause trouble tend to present with menorrhagia and/or dysmenorrhoea. Leiomyomas can also cause
dyspareunia.
Large leiomyomas can be associated with symptoms due to their sheer bulk, such as pelvic pain. Compression of the bladder and/or rectum can result in urinary frequency or obstruction, or constipation or pain on defaecation.
Leiomyomas may cause infertility due to distortion of the uterine cavity, although infertility is not a typical presentation or common complication.
Very rarely a leiomyoma can increase the levels of erythropoietin in the blood and induce polycythaemia.
During pregnancy red degeneration of a fibroid presents as pelvic pain, possibily accompanied by fever. Large fibroids can result in the fetus adopting an abnormal position in the uterus as term approaches and this may make vaginal delivery awkward. A large fibroid can theoretically cause obstructed labour. Post partum haemorhage may occur.
Fibroids may be palpable on bimanual examination.
Investigations
The presence of leiomyomas can be diagnosed by ultrasound. However, given that patients tend to present with menorrhagia it is prudent to perform a full blood count to determine if the patient is anaemic. The degree of menorrhagia may also have been exacerbated by a coagulation disorder, so clotting studies are prudent; the full blood count will also assist in this regard by disclosing the platelet count.
Treatment
Whether or not treatment is given will depend upon the severity of the symptoms. NSAIDs can alleviate dysmenorrhoea in many instances. Menorrhagia may be amenable to a progesterone-releasing IUCD.
Agonists of gonadotropin-releasing hormone can be given by injection. Although these cause an initial surge in the levels of oestrogen and progesterone the long term effect is to reduce the levels and this deprives the fibroids of their hormonal nourishment.
Danazol is an alternative drug that can induce the regression of fibroids, although it has androgenic side effects that make it unpopular.
Embolisation of the branches of the uterine artery that supply the leiomyomas can be attempted, as can radiofrequency ablation of the lesions.
While hysterectomy is curative of uterine fibroids, it also renders the patient effectively infertile. This can be problematic in that leiomyomas tend to be symptomatic only in the child-bearing years. Nevertheless, if the lady has completed her family hysterectomy is an effective treatment for troublesome fibroids.
Myomectomy is an alternative surgical technique in which only the leiomyomas are removed from the uterus. In some patients this can generate a specimen that contains over twenty fibroids.