Contents
Introduction
Oedema is the presence of excess fluid within the extracellular space. Oedema is a feature of various diseases and is best understood by considering the mechanisms that govern the normal distribution and movements of fluids.
Normal Fluid Distribution and Movement
Approximately 70% of body weight is contributed by water. This water is distributed in three compartments.
- Intravascular (7%)
- Intracellular (66%)
- Intercellular (27%)
The intravascular and intercellular compartments are together referred to as the extracellular compartment.
The intercellular compartment is also known as the interstitial. It includes a subcompartment, specialised fluids, that accounts for 2% of total body water. The specialised fluids compartment is formed by secretions of the GI tract, peritoneal and pleural fluids, cerebrospinal fluid, synovial fluid, intraocular fluid and the vestibulocochlear fluids.
In absolute terms, the intravascular volume may be estimated from the principle that there are 70ml of blood for every 1kg of body weight.
The separation between the compartments is achieved by cell membranes and intercellular junctions. These constitute partial or complete barriers to the movement of water. Their permeability can be increased by the insertion of small channels that allow the passage of water, pores and relaxation of the junctions.
Hence, the compartments are not isolated boxes. Instead, they constitute a dynamic distribution in which there is constant movement between the three locations. This movement occurs by various processes.
- Passive diffusion along a concentration / osmotic gradient
- Passive diffusion along a pressure / hydrostatic gradient
- Ion pumps
Ion pumps move ions, often against a gradient, between the intracellular and extracellular compartments. Redistributing ions in this way can generate concentration gradients that cause water to move in the same direction as the ions. This process assists the absorption of water in the gastrointestinal tract and drags water into various secretions, such as sweat.
The main intracellular cation is potassium. The principle extracellular cation is sodium. This ionic distribution is the basis of the electrical activity of excitable cells like neurones.
In terms of anions, chloride dominates in the extracellular compartment while negatively charged proteins supply the intracellular anionic component; the attendant chloride gradient is utilised by neurones to inhibit electrical activity.
The Capillary Bed
The capillary bed is the part of the blood system in which transfer of gases, fluid and nutrients between the tissues and the blood occurs. Capillaries are fed by arterioles (which are themselves supplied by arteries) and drain into venules, which in turn connect to veins. They form a dense network within the tissues.
The wall of capillaries is formed only by endothelial cells. The endothelial cells are connected by intercellular junctions that are permeable to water and small molecules (for example glucose and amino acids) and therefore allow these substances to move between the blood and the tissues. The direction of movement of chemical substances follows concentration gradients, while that of water is determined by the hydrostatic pressure and the oncotic pressure.
The hydrostatic pressure is a result of the blood pressure that is necessary to permit blood flow. The hydrostatic pressure within the blood vessel forces fluid out of the lumen of the blood vessel into the interstitial compartment (the water pressure inside a garden sprinkler is an anology).
The oncotic pressure is produced by plasma proteins that are too large to move through the spaces between the endothelial cells. These proteins provide an osmotic effect that retains water within the capillary or causes draws it from the interstitial compartment into the intravascular compartment.
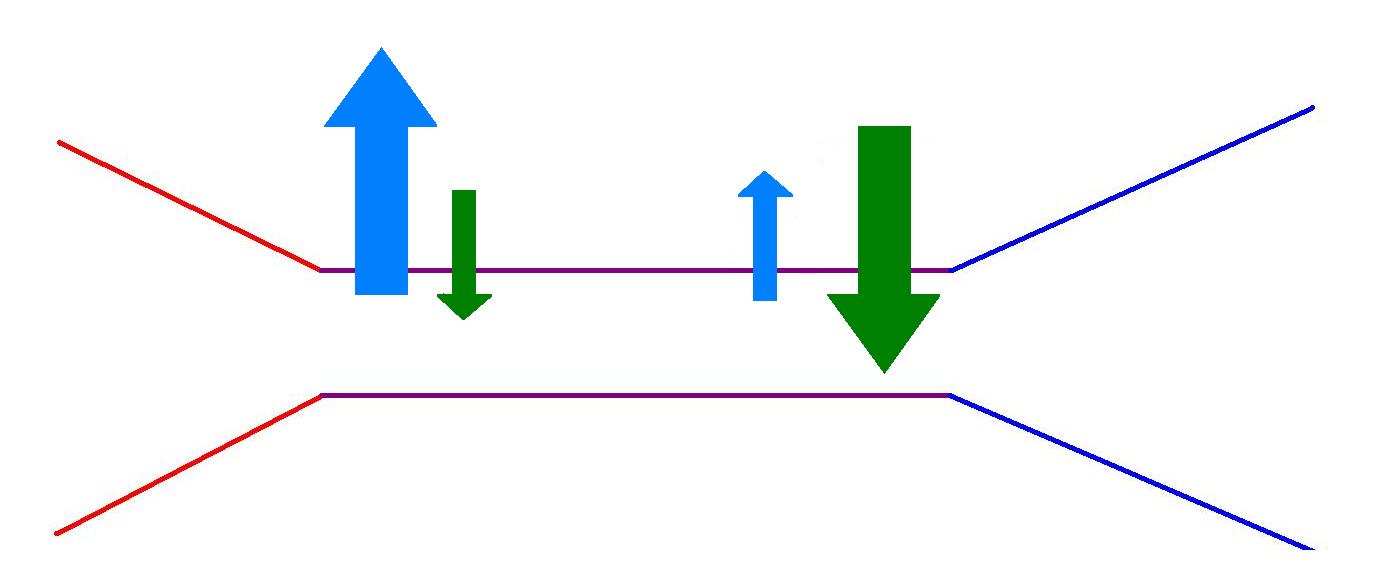
On the arterial side of the capillary bed the hydrostatic pressure exceeds the oncotic pressure and there is a net movement of water from the capillaries into the extravascular space. On the venous side of the capillary bed, the hydrostatic pressure has fallen a little and the loss of water has increased the oncotic pressure such that the balance between the two has shifted to favour the net movement of water back into the blood.
|
|
On the arterial side (red) of the side of the capillary bed, the hydrostatic pressure (light blue) exceeds the effect of the opposing oncotic pressure (green). At the venous side (mid blue) the hydrostatic pressure has fallen and the oncotic pressure dominates.
|
Lymphatics
A small volume of the water that leaves the blood vessels on the arterial side of the capillary bed is not reclaimed on the venous side. This excess is drained from the tissues by the lymphatic channels. The lymphatics are a network of endothelial-lined, thin walled vessels that ultimately drain back to the thoracic duct, which itself drains into the left brachiocephalic vein, thus returning lymphatic fluid to the circulating blood volume. The lymphatic channels pass through lymph nodes on the way to the thoracic duct. The fluid within the lymphatics is known as lymph and has a white colour.
Oedema
Oedema occurs when the balance of the diffusion of water between the intravascular and interstitial spaces shifts in favour of the latter and excess fluid accumulates in the extracellular space until a new equilibrium is attained. This shift can be generated by several mechanisms.
- Increased capillary permeability
- Increased venous pressure
- Reduced plasma oncotic pressure
- Impaired lymphatic drainage
The intercellular junctions between endothelial cells can be modulated to enhance their permeability. This may involve the simple process of a contraction of the endothelial cells to increase their spacing. As well as allowing easier movement of water, the elevated permeability permits some plasma proteins to leave the capillaries, thereby dispersing some of the oncotic pressure. Increased capillary permeability is the main mechanism of oedema in
acute inflammation. In the case of acute inflammation the oedema is an intentional event with the intention of having a net benefit.
If the pressure in the venous part of the vasculature is raised, this will be transmitted back to the capillary bed and the increased hydrostatic pressure will promote the movement of fluid into the tissues from the blood, as well as reducing fluid reclamation in the venous side of the capillary bed. Elevation of the venous pressure occurs in low output cardiac failure due to the inability of the heart to keep up with the rate of venous return to it.
A fall in the plasma oncotic pressure will reduce the osmotic gradient that favours the movement of water into the blood from the tissues. Plasma oncotic pressure drops if there is either an abnormally high rate of loss of protein from the body (such as nephrotic syndrome) or a failure to make sufficient quantities of plasma proteins (cirrhosis) or in protein malnutrition.
Partial or complete blockage of the lymphatic drainage of part of the body prevents the drainage of lymph and removal of the normal quantity of excess fluid that naturally results from fluid balance at the capillary bed level. Lymphatic obstruction can be a consequence of surgical removal of a group of lymph nodes or infections such as filariasis.
An elevation of arterial pressure (hypertension or high blood pressure) does not cause oedema because the elevated arterial pressure has usually dissipated by the time the capillary bed is reached.
Retention of excess sodium and water is seldom sufficent on its own to produce oedema.
Effusions
The processes that give rise to oedema can also cause the accumulation of effusions within body cavites such as the pleura and peritoneal cavities. Fluid within the peritoneal cavity is known as ascites.
A
transudate is an effusion that has a low protein content. Transduates are usually the result of elevations in venous pressure or reductions in plasma oncotic pressure.
An
exudate is an effusion that has a high protein content. Exudates reflect oedema secondary to an inflammatory process.