Contents
Introduction
Sympathetic Nervous System
Parasympathetic Nervous System
Introduction
The autonomic nervous system controls basic bodily functions that are regulated at an unconscious level. It is divided into two components, the
sympathetic and the
parasympathetic. The main role of the sympathetic nervous system is to activate and stimulate the body for the fight or flight response whereas the parasympathetic nervous system has a more calming role. The actions of the two systems at any given target organ tend to be complementary, although some organs, particularly blood vessels, receive innervation from only one of the two components.
The central processing for the autonomic nervous system occurs mainly in the brainstem, assisted by other evolutionarily old parts of the brain such as the hypothalamus. The brain's autonomic processing centres receive sensory information via peripheral nerves (both autonomic and somatic) and have dedicated motor / effector autonomic output nerves. The anatomy of the autonomic nerves differs between the sympathetic and parasympathetic systems, as does the neurotransmitters they employ.
Sympathetic Nervous System
The sympathetic nervous system stimulates the body for action such as fight or flight. Examples of the effect of the sympathetic nervous system are as follows.
|
Heart
|
Increases heart rate
Increases the strength of cardiac contraction
Increases the tendency of cardiac myocytes to depolarise without external input (automaticity)
|
|
Blood vessels
|
Vasoconstriction when alpha-1 adrenoreceptors are present
Vasodilatation when beta-2 adrenoreceptors are present
|
|
Lungs
|
Bronchodilatation
|
|
Energy Metabolism
|
Increases glycogenolysis in the liver
Increases glucagon release from the pancreas
Reduces insulin releases from the pancreas
Stimulates lipolysis in fat
In general makes glucose and fat available for energy
|
|
Eyes
|
Dilates pupil
Focuses the eye for distance vision
|
|
GI Tract
|
Decreases peristalsis
Contracts sphincters
|
|
Bladder
|
Constricts sphincter
Relaxes the detrusor muscle of the bladder
|
|
Skin
|
Increases sweating
Contracts erector pili muscles (makes hairs stand on end)
|
|
Uterus
|
Contracts uterine smooth muscle when acting via alpha adrenoreceptors
Relaxes uterine smooth muscle when acting via beta adrenoreceptors
|
Many of the above functions are co-operative. The heart is stimulated to increase cardiac ouput. Airflow into the lungs is improved to meet an increased demand for oxygen. Glucose and fatty acids are mobilised from their respective reserve stores in the liver and adipose tissue so that they are available for the skeletal muscles, heart and brain. The GI tract and bladder are put into a dormant state in order to reduce their metabolic and blood flow requirements. Dilatation of the pupil allows more light to enter the eye which improves sensitivity to movement (although at the expense of a loss of fine detail) and the lens shifts to distance vision to detect incoming attacks.
Anatomy
The nerves of the sympathetic nervous system leave the spinal cord in the spinal nerves of all twelve thoracic segments of the spinal cord, plus first to second or third lumbar segments (T1-L2/L3).
The sympathetic nervous system uses a two nerve pathway to send a signal from the brain to the target cell. The first neurone in this short chain is called the
preganglionic cell and the second neurone in the pathway, which relays the signal on from the first cell to the target itself, is known as the
postganglionic cell.
The synapse between the preganglionic and postganglionic neurones occurs in one of the
sympathetic ganglia; a ganglion is a collection of nerve cell bodies.
Many of the sympathetic ganglia are located in the paravertebral sympathetic chain which is situated on either side of the vertebral column and extends from the neck to the coccyx. Given that the outflow of sympathetic nerves from the spinal cord only emerges from T1-L2/L3, some preganglionic fibres have to travel up or down a considerable distance to reach their target ganglion.
The upper end of the chain features three cervical ganglia, the superior, middle and inferior. The superior is the largest, the middle is the smallest and the inferior is sometimes called the stellate ganglion if it is fused with the first thoracic sympathetic ganglion. The middle and inferior cervical ganglia provide sympathetic innervation to the heart.
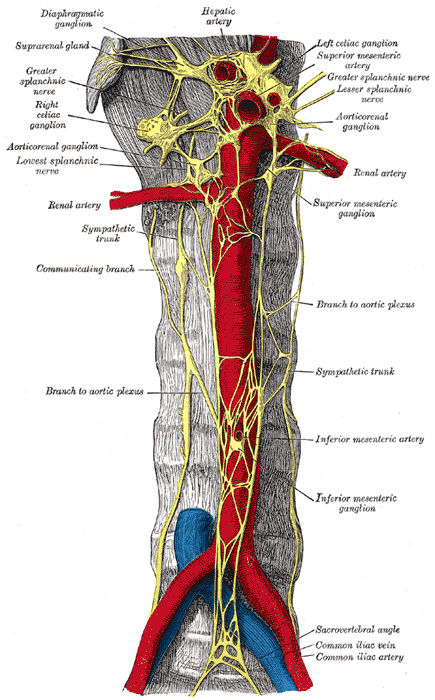
Not all preganglionic fibres synapse with their postganglionic cell in the paravertebral ganglia. Instead, some sympathetic ganglia are situated in front of the vertebral column (prevertebral ganglia). These ganglia are associated with the three main blood vessels that supply the GI tract and hepatobiliary system and derive their names from these vessels, thus giving the coeliac, superior mesenteric and inferior mesenteric ganglia. They supply sympathetic innervation to the GI tract.
|
Prevertebral Sympathetic Plexus
Image courtesy of Wikipedia
|
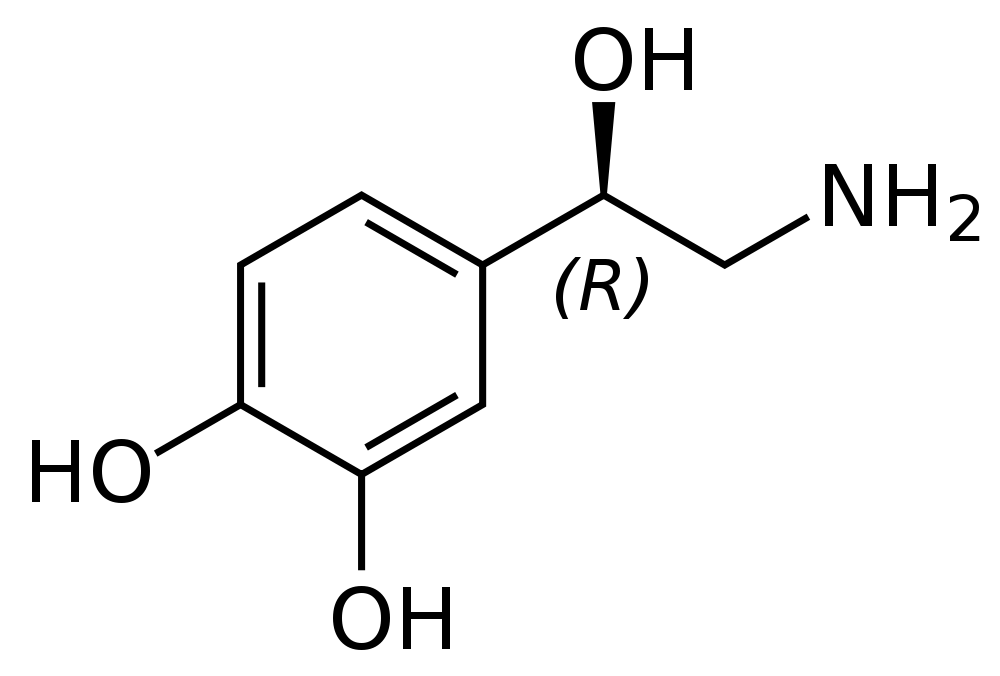
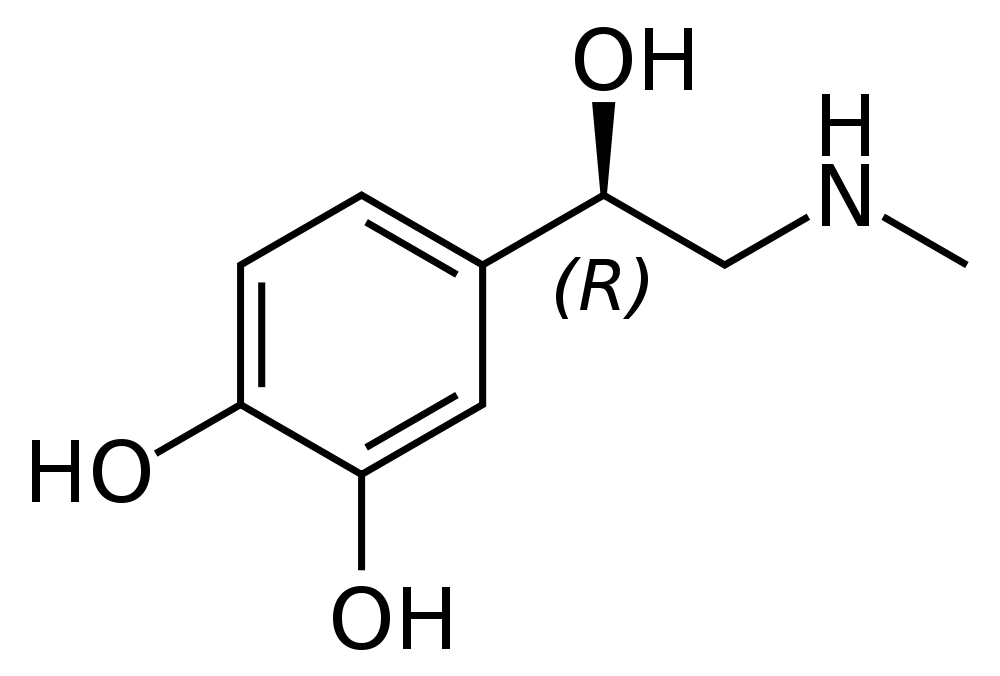
Adrenal Medulla
The medulla of the adrenal gland is a bonus feature of the sympathetic nervous system. No equivalent structure exists for the parasympathetic nervous system. The adrenal medulla synthesises noradrenaline and adrenaline, which are collectively known as catecholamines. Both adrenaline and noradrenaline can stimulate the adrenoreceptors used by postganglionic sympathetic fibres to communicate with their target cells. The medulla of the adrenal gland releases adrenaline and noradrenaline into the blood and therefore provides a systemic boost to the sympathetic nervous system across multiple organs; direct stimulation of organs by postganglionic sympathetic nerves can be targeted to specific organs. Adrenaline release dominates over noradrenaline by a ratio of around 6 to 1.
The adrenal medulla is innervated by preganglionic sympathetic fibres. No postganglionic axons are involved. The catecholamine-producing cells of the adrenal medulla are derived from embryological neuronal precursors. These precursors cells undergo a special pathway of differentiation that restricts them to synthesising catecholamines without expressing the axons and dendrites.
|
|
Noradrenaline
Image courtesy of Wikipedia
|
Adrenaline
Image courtesy of Wikipedia
|
Neurotransmitters and Receptors
The sympathetic nervous system has a limited array of neurotransmitters and receptors.
The preganglionic fibres release acetylcholine. This acts on
nicotinic cholinergic receptors on the postganglionic cell (including the cells of the adrenal medulla).
With one exception, the postganglionic cells employ noradrenaline as their neurotransmitter. This binds to adrenoreceptors, of which there are five different types, alpha-1, alpha-2, beta-1, beta-2 and beta-3.
Alpha-1 adrenoreceptors are found mainly on smooth muscle. They induce contraction of smooth muscle and are involved in vasoconstriction and the closure of the spincters of the bladder and the anus. The alpha-1 adrenoreceptor is coupled with a G protein-phospholipase C second messenger system.
Alpha-2 adrenoreceptors have similar post-synaptic effects to alpha-1 adrenoreceptors although are minor players compared with alpha-1. However, they also participate in the regulation of synpatic activity by the fact that they are found on the presynpatic part of an adrenergic synapse and can therefore modulate the behaviour of the presynpatic terminal in response to activity at the synpase. They may also be involved in other aspects of CNS neurotransmission. Alpha-2 adrenoreceptors use the G protein adenylate cyclase second messenger system.
Beta-1 adrenoreceptors are also coupled to the adenylate cyclase system. They are found in the heart and the juxtaglomerular apparatus of the kidney. In the heart they mediate the positive inotrophic and chronotropic effects of the sympathetic nervous system. Their action of the juxtaglomerular apparatus is to stimulate the release of renin.
Beta-2 adrenoreceptors are another associate of the adenylate cyclase system. Their distribution centres on the smooth muscle of blood vessels, bronchi, GI tract, bladder and uterus. They have the opposite effect to alpha-1 adrenoreceptors and relax smooth muscle. This phenomenon provides an example of how one signal (a catecholamine) can have different effects depending on the second messenger system employed by the target organ. In addition, adrenaline is considerably more potent than noradrenaline on beta-2 adrenoreceptors. The blood vessels of skeletal muscle are dominated by beta-2 rather than alpha-1 adrenoreceptors and therefore vasodilate in response to an increase in sympathetic activity, as would be appropriate in a fight or flight situation that requires a lot of skeletal muscle contraction.
Beta-3 adrenoreceptors are the most recently discovered member of the team. They are present on adipose tissue and skeletal muscle and induce lipolysis and skeletal muscle thermogenesis.
The exception to the adrenergic pattern of postganglionic sympathetic nerves is the innervation of sweat glands. These postganglionic sympathetic fibres employ acetylcholine which acts on muscarinic receptors.
Parasympathetic Nervous System
The parasympathetic nervous system calms the body down and allows it to take things easy. Examples of actions of the parasympathetic nervous system are as follows.
|
Heart
|
Decreases heart rate
|
|
Blood vessels
|
Ineffective in most blood vessels but can vasodilatate blood vessels that supply erectile tissue
|
|
Lungs
|
Bronchoconstriction
|
|
Energy Metabolism
|
Deceases glucagon release from the pancreas
Increases insulin secretion from the pancreas
|
|
Eyes
|
Constricts pupil
Focuses the eye for near vision
Promotes the production of tears
|
|
GI Tract
|
Stimulates the secretion of large volumes of watery saliva
Promotes the secretion of gastric acid
Increases the quantity of fluid and mucus secreted by the glands of the small and large bowel
Increases peristalsis
Relaxes sphincters
|
|
Bladder
|
Relaxes sphincter
Contracts the detrusor muscle of the bladder
|
The range of actions of the parasympathetic nervous system is less than that of the sympathetic. The skin and uterus are not influenced by the parasympathetic nervous system while the effects on the heart are limited to heart rate whereas the sympathetic nervous system affects both heart rate and the strength of myocardial contraction. The actions of the parasympathetic nervous system on energy metabolism are the opposite to those of the sympathetic: the parasympathetic nervous system promotes an anabolic state by stimulating the release of insulin from the pancreas while the sympathetic nervous system shifts the body into a state of lipid and carbohydrate catabolism in order to supply energy substrates to the skeletal muscle. However, the sympathetic system influences more target tissues to achieve its goal.
The parasympathetic nervous system has one of its strongest associations with the GI tract and the process of digestion. The secretion of saliva is stimulated to facilitate mastication and initiate digestion. The production of gastric acid is increased, as are the secretions of the small and large bowel. Having primed the GI tract to receive the meal, the parasympathetic nervous system also invigorates the smooth muscle of the GI tract to undertake mechanical digestion and movement of the meal.
The absence of parasympathetic opposition to some elements of sympathetic function, such as vasonconstriction and the positive inotropic action on the heart, may seem odd as there would appear to be no way to challenge the actions of the sympathetic nervous system. However, control is provided by withdrawing the sympathetic drive to the heart and vascular smooth muscle. If the sympathetic stimulation is removed, myocardial contraction reduces in strength and vascular smooth muscle relaxes. Indeed, ineffective function of the sympathetic nervous system features hypotension, particularly on standing up, because vasoconstriction cannot be triggered in vascular smooth muscle.
Anatomy
The parasympathetic nervous system uses a rather different array of nerves to the sympathetic. The nerves which carry parasympathetic fibres are the third, seventh, ninth and tenth cranial nerves and the second to fourth sacral spinal nerves.
The third cranial nerve (oculomotor) includes the parasympathetic fibres which constrict the pupil and contract the ciliary muscle (which causes the eye to focus for near vision).
The seventh cranial nerve (facial) provides the parasympathetic innervation for the lacrimal gland, submandibular salivary gland and the sublingual salivary gland. In order to reach their targets, these fibres end up hitching a ride with branches of the fifth cranial nerve (trigeminal).
The glossopharyngeal nerve has branches which supply the parasympathetic innervation of the parotid gland.
The tenth cranial nerve (vagus nerve) probably has grounds for making some sort of complaint on the basis of a misleading job description. Despite being a cranial nerve the vagus nerve has to cover a large amount of territory. In addition to its somatic motor innervation of the pharynx and larynx, the vagus nerve also bears the parasympathetic fibres that supply the heart, lungs, oesophagus, stomach, pancreas, small intestine and the colon as far as the splenic flexure.
The second, third and fourth sacral spinal nerves contain the parasympathetic fibres which innervate the colon distal to the splenic flexure, the bladder and the genitalia.
Like the sympathetic nervous system, the parasympathetic nervous system employs the preganglionic-postganglionic two neurone pathway for the innervation of its target tissues. However, in contrast to the sympathetic nervous system the parasympathetic ganglions are usually close to their target tissue. In the case of the sacral outflow, the ganglia are actually situated in the walls of the target organs and so the postganglionic fibres are very short.
There are four cranial nerve parasympathetic ganglia, the ciliary (fibres for the eye), otic (located in the ear but actually has the fibres for the lacrimal, sublingual and submandibular glands, submandibular (sublingual and submandibular glands) and pterygopalatine (parotid gland).
Neurotransmitters and Receptors
The parasympathetic nervous system is devoted to acetycholine and will settle for nothing else at either its preganglionic or postganglionic synapses. However, acetylcholine likes a bit of variety, not only because it is found in other parts of the nervous system beyond the autonomic but because even within the autonomic system it enjoys flirting with different receptors.
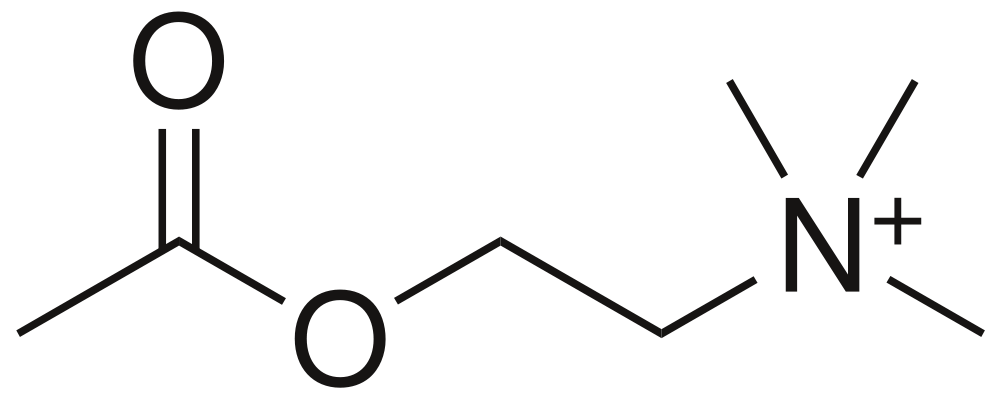
|
Acetylcholine
Image courtesy of Wikipedia
|
The preganglionic synapse has nicotinic receptors for the acetylcholine. The postganglionic synapses employ muscarinic receptors. Three subtypes of muscarinic receptors exist in the parasympathetic system (M
1, M
2 and M
3); subtypes M
4 and M
5 have been described in the central nervous system.
The M
1 receptors are present in salivary glands and on the acid-producing gastric parietal cells. It is mainly associated with the phospholipase C second messenger system.
M
2 receptors are found in the heart. Unlike the other two types of autonomic muscarinic receptors their effects are mediated by adenylate cyclase and cyclic AMP.
M
3 receptors have a far more general distribution that includes the smooth muscle of the GI tract, bronchi, pupil, ciliary body, salivary glands and GI glands. They are coupled to the phospholipase C second messenger system.