Introduction
Several different types of histopathological specimens can be obtained from the breast. In general the cut up of breast specimens follows the principles of the cut up of the tumour of a
solid organ; breast specimens are in some respects the archetypal model of a solid organ.
Biopsy
Breast core biopsies are handled as for other types of core biopsies and are transferred from the pot to cassette after counting their number and measuring their size range. In some hospitals the biopsies are placed into cages or cassettes at source.
Biopsies that are taken for microcalcification are typically obtained under radiological guidance and are X-rayed before they are sent to the histopathology department in order to check that the biopsies contain calcification. A copy of this plain X-ray may be provided.
Some small lesions may be removed by mammotome biopsy in which repeated cores are taken through the lesion in order to excise it from the breast in a piecemeal fashion. The histopathological examination cannot comment on the excision status in such cases.
Lumpectomy / Narrow Local Excision
The term lumpectomy can be applied to a variety of breast specimens which span the territory between a core biopsy and a mastectomy (excluding these two ends of the spectrum). However, for the purposes of discussion here it is used to denote removal of a relatively small portion of the breast that contains the lesion and only a narrow rim of normal breast tissue. Such specimens are employed to remove benign lesions or lesions that are of uncertain nature but which are unlikely to transpire to be malignant. This narrow local excision approach conserves breast tissue and reduces the likelihood of problems of asymmetry arising after the procedure.
A narrow local excision should be measured in three dimensions and weighed. Opinion is divided on whether or not the surface should be inked but marking the surface in this fashion can avoid uncertainty as to where the excision margin is should the specimen be discovered to contain a malignant tumour.
The specimen should be serially sliced at narrow intervals and the cut surface described. The appearance of the cut surface can be compared with that expected from the clnical details (if these contain sufficient information or reference to the pre-operative diagnosis).
Further debate exists as to whether the specimen should be embedded in its entirety or not. Tumours such as fibroadenomas rarely exceed 30mm so complete embedding should not generate an excessive number of blocks, although some pathologists still prefer sampling. Larger specimens may make automatic complete embedding impractical. If sampling is to be undertaken the blocks should demonstrate the spectrum of the features of the cut surface, as well as the margin. The standard concept of at least one block per centimetre can be a useful guide.
If the narrow local excision is performed for a lesion that has either a risk of malignancy and/or for microcalcification, complete embedding may be essential to ensure that the lesion has been demonstrated.
Wide Local Excision
Wide local excisions are usually reserved for malignant tumours. In order to be suitable for a wide local excision the tumour should be small in relation to the size of the breast. The tumour will also usually need to be unifocal within the breast.
The purpose of a wide local excision is to excise the malignant tumour with an adequate margin while conserving the rest of the breast and reducing the need for reconstruction.
Wide local excision specimens are usually orientated by means of sutures and/or marker clips. Some hospitals have standard protocols for how the markers should be applied and in such situations the meaning of the markers may not be reiterated on the request form. Underlying the process of orientation is the approximation of the specimen to a cuboid.
The majority of wide local excisions do not have attached skin.
Orientated wide local excision specimens should be differentially inked. Six colours is ideal, although the orientation can be preserved with only five colours because two of the six faces of the wide local excision will be the first and last slices and therefore cannot be in the same block (fewer than five colours can theoretically permit orientation but requires careful tracking of the slices as they are handled and is therefore more susceptible to error).
A wide local excision is normally sliced in the parasagittal planes (from medial to lateral or from lateral to medial). However, there be some situations, such as the presence of a guide wire, that make slicing in the transverse planes a better option (from superior to inferior or vice versa) (rarely a pathologist may prefer to slice in the coronal planes, from superficial to deep or vice versa). This decision must be made before inking if less than six different colours of ink are to be employed because it is necessary to determine which faces will form the ends of the specimen and can therefore be inked the same colour.
A wide local excision specimen should be measured in three dimensions. The orientated nature of most wide local excisions means that the measurements can be given anatomical designations (top to bottom, side to side, front to back). The specimen should be weighed.
The specimen should be divided into parallel slices. If possible, the slices should be sufficiently thin that they are no thicker than can be contained in a standard cassette. The number of slices should be stated, as well as which anatomical aspects of the specimen the first and last slice contain.
A wide local excision will usually contain only one lesion, although it is important to remain alert to the possibility of more than one tumour. The size of the tumour should be measured in three dimensions (one of which will be across the involved slices); these dimensions can be related to the same anatomical designations as the size of the whole specimen. The slices of the specimens that contain the tumour should be stated. The distance of the tumour from the six margins (lateral, medial, superior, inferior, superficial and deep) should be given. The appearance of the tumour should be described.
The blocks should demonstrate the nature of the tumour and its relationship to all six margins. Four of these margins will be present in the slices that contain the tumour; the two end margins will usually not be (typically the medial and lateral margins). These two end margins can be checked by embedding the first and last slice. For larger wide local excisions it may not be possible to include both the tumour and the margins in the same slice in the same cassette. Either a megablock can be employed or the aspect of the margin closest to the tumour can be sampled separately.

|

|
|
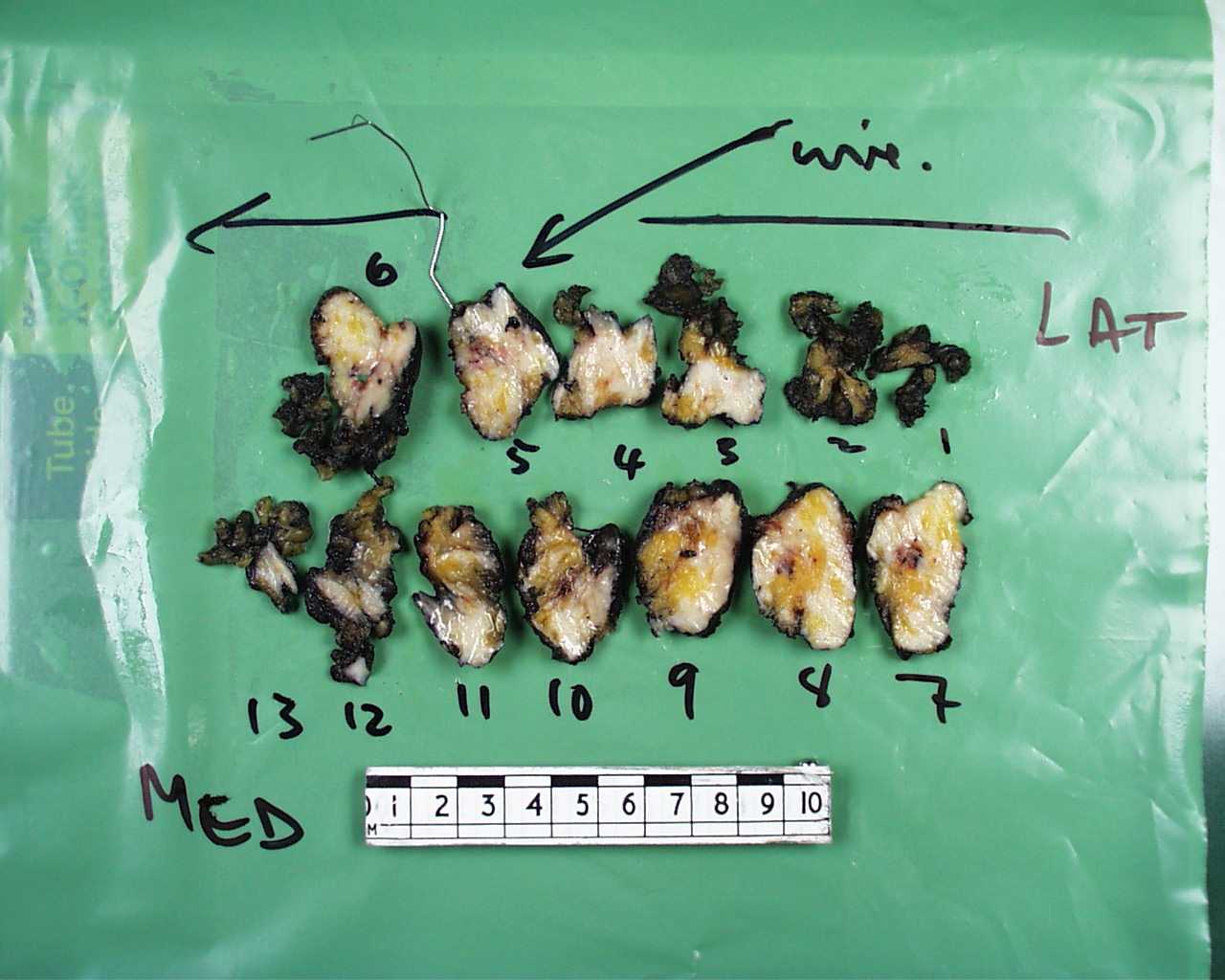
An example of a wide local excision. Unusually this has only been inked in one colour. The lesion is present in the second slice from the right in the bottom row.
|
A slice from a wide local excision that included an ellipse of skin. The margins have been inked with different colours.
|
An example description for a breast wide local excision specimen is as follows.
The specimen comprises a portion of fibrofatty tissue that measures 50mm superiorly to inferiorly, 40mm from medial to lateral and 25mm from superficial to deep. The weight of the specimen is 90g.
Three sets of orientating sutures are present and are compatible with the stated orientation.
The specimen has been divided from medial to lateral into nine slices, with the medial slice being slice one. Located in slices four, five and six is a firm, white, irregular tumour that measures 15mm by 12mm by 12mm (vertical by medial to lateral by superficial to deep). The tumour is 10mm from the superior margin, 25mm from the inferior margin, 15mm from the medial margin, 13mm from the lateral margin, 6mm from the superficial margin and 7mm from the deep margin.
The medial margin has been inked blue, the lateral margin inked green, the superior margin inked red, the inferior margin inked yellow, the superficial margin inked orange and the deep margin inked black.
A1+A2) Medial margin (slice 1)
A3+A4) Lateral margin (slice 9)
A5) Tumour and superior margin (slice 5)
A6) Tumour and deep margin (slice 5)
A7) Tumour and superficial margin (slice 5)
A8) Tumour (slice 4) (no margins)
A9) Tumour (slice 6) (no margins)
A10) Inferior margin (slice 6)
A11) Breast away from the tumour (slice 2)
In the above example, if only five colours of ink had been available the medial and lateral margins would have been inked the same colour.
Wire Guided Specimens
Some breast lesions are discernible radiologically but are not palpable. In order to allow the surgeon to remove these lesions by either a narrow local excision or wide local excision a wire may be inserted into the lesion under radiological guidance.
When cutting up a wire guided specimen consideration should be given to slicing the specimen parallel to the wire (provided that the wire is approximately in a vertical or horizontal plane). This will limit the number of cuts that have to be made around the wire (alternatively some form of wire cutters can be used to extricate the wire). However, whatever approach is adopted to negotiate the presence of the wire it is vital not to dislodge the tip until the slice (or slices) it occupies is determined. A lesion may or may not be visible in these slices. If a lesion is visible the cut up can proceed as for a standard narrow local or wide local excision. If not lesion is identifiable then all slices containing the tip of the needle should be embedded, plus the slice on either flank of this region and the slices that secure the end margins.

|
|
|
A wire-guided narrow local excision
|
The same specimen divided into slices. Note how the division into slices has been made so as to restrict the wire to penetrating just one slice.
|
Mastectomy
A mastectomy is the removal of the entire breast, including the axillary tail. A mastectomy is usually accompanied by removal of the axillary lymph nodes. These may or may not be in continuity with the main specimen.
Some mastectomies are 'skin sparing' in which only a small portion of skin from the centre of the breast, bearing the nipple, is removed; in other mastectomies the skin covers most of the specimen.
The ellipse of skin should be measured in transverse and vertical dimensions. The presence or absence of the nipple should be stated. The appearance of the nipple should be recorded.
The underlying fibrofatty tissue is measured in three dimensions. If the axillary lymph nodes are attached these should be measured separately.
The mastectomy should be weighed.

|
 |
|
A mastectomy and attached axillary lymph node dissection
|
A skin sparing mastectomy without attached axilluar dissection
|
The surface of the fibrofatty tissue is inked. Usually one colour is sufficient.
The mastectomy is sliced in the parasagittal plane (variation on this is very rare). The cuts of the slices usually do not go through the skin and thus the slices are in effect hinged on the skin. The slices and any lesions they contain are approached in the same way as those for a wide local excision.
In a standard mastectomy there is no superficial margin; instead the skin constitutes a superficial surface. In a skin-sparing mastectomy the superficial aspect of the specimen may be either a margin (if fibrofatty tissue) or a surface (if covered by the small ellipse of skin); in either case the position of the tumour relative to the superficial aspect is still measured.
The tumour is blocked using the same approach as for a wide local excision specimen. Most of the margins will be too far away from the tumour to include the tumour in the same block as the margin.
Once the tumour or tumours have been sampled, one block should be taken from each of the four quadrants of the breast, aiming to sample fibrous tissue rather than fat. At least one block of the nipple should be taken even if the nipple looks normal.
A few lymph nodes may be found in the lateral end of the specimen even if an axillary dissection is not attached so it is prudent to search for lymph nodes in the most lateral slices.
|

|
|
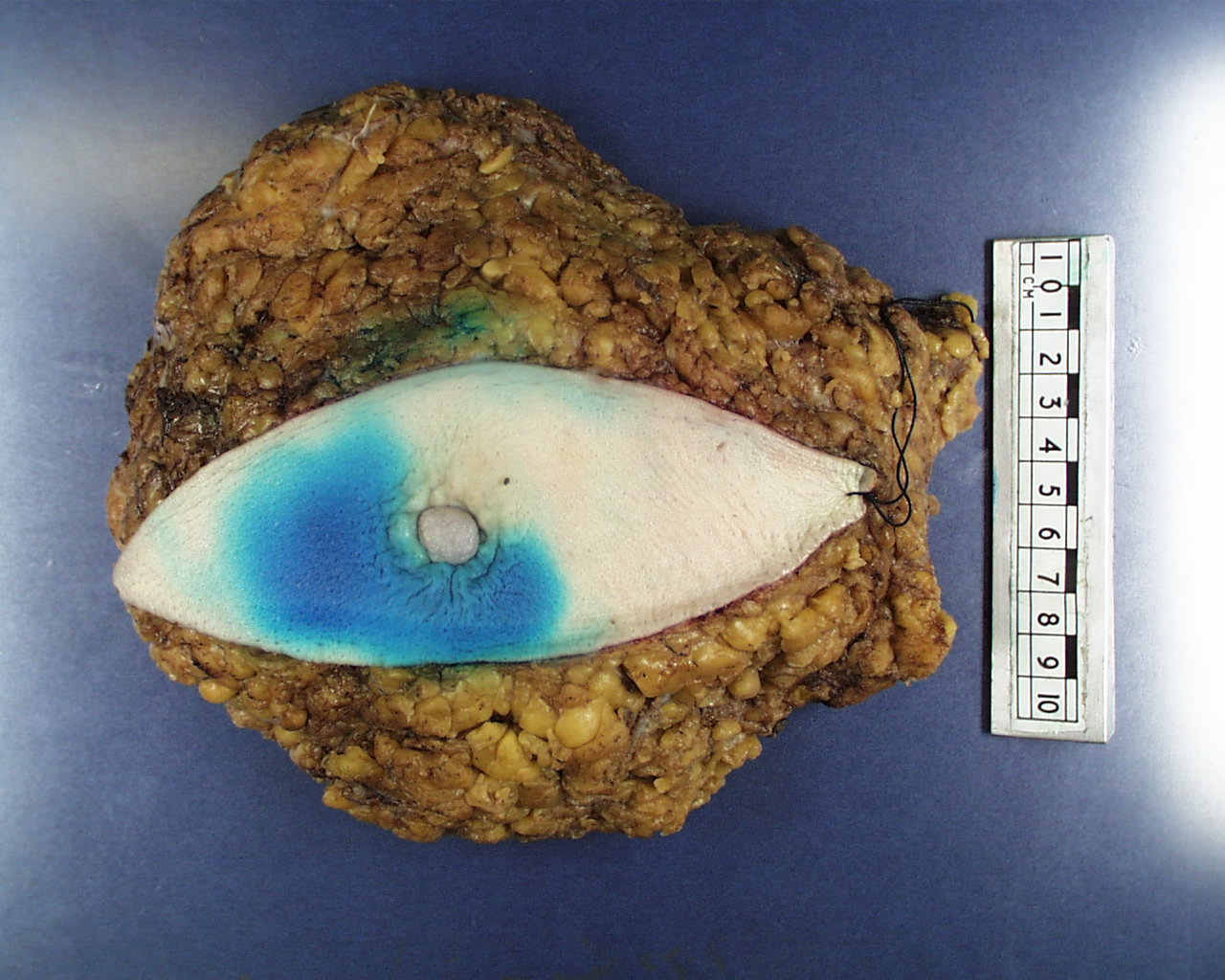
A mastectomy without axillary dissection. The blue dye is one of the tracers used in the detection of the sentinel lymph node(s)
|
The same mastectomy viewed from the deep surface after slicing. A grey-white tumour is present in the two everted slices.
|
An example of the opening of the description of a mastectomy specimen is as follows.
The specimen comprises an ellipse of nipple bearing skin and underlying fibrofatty tissue that weighs (weight in grams). The ellipse of skin measures x1 by y1 millimetres. The underlying fibrofatty tissue measures x2 by y2 millimetres by z2 millimetres in thickness. The attached axillary dissection measures x3 by y3 by z3 millimetres.
The nipple appears (insert description here, typically normal / inverted / retracted / distorted / irregular).
Specimen X-rays
Wide local excision specimens are often x-rayed to check that they contain the lesion. This x-ray may be supplied to the pathologist. Sometimes it is necessary to x-ray the slices of a wide local excision or a mastectomy in order to locate the lesion(s) and allow only the relevant slices to be embedded, as opposed to embedding a much greater proportion of the specimen.
Breast Reduction
Breast reduction surgery is performed either for cosmetic reasons or to address asymmetry that occurred after unilateral surgery for neoplasia or to provide relief from mechanical back pain. Tissue is usually received from both breasts. Gender reassignment will typically involve a bilateral mastectomy.
Breast reduction specimens tend to come in the form of several or more pieces of tissue, at least some of which will have overlying skin. While each piece is measured in three dimensions the most important measurement is the weight. Should a dispute arise in the future with regard to the cosmetic result documentation of the mass of tissue removed from each side can be useful in resolving the situation.
Each piece of tissue should be sliced and inspected for abnormalities. The pre-operative work up of the patient should have made this unlikely. If no abnormalities are seen only around six blocks are taken from the total tissue from each breast (local protocoals and the nature of individual specimens will affect this number). If an abnormality is present then it is blocked as for a focal lesion in either a local excision or mastectomy.

|
|
An example of a breast reduction
|