Contents
Introduction
Hollow organs are one half of the dichotomy that is completed by solid organs. In simple terms, the former are tubes and the latter are cubes.
Not surprisingly, tube is an oversimplification and the colloquial description is better offered as tubes and bags.
Common to all hollow organs is anatomy which consists of a lumen and a surrounding wall. The lumen may either be open at both ends of the specimen(tube) or be closed at one end (bag).
The tubular hollow organs of the body encompass the GI tract and therefore the oesophagus, stomach, small intestine and large intestine. The larynx can also be added to this list. Resection of any of these organs will yield a tube.
The bag hollow organs include the bladder, uterus and gallbladder. Each of these is closed at one end (ureters in the case of the bladder and fallopian tubes for the ureter excluded).
The hollow organs of the body typically have four layers (from the inside out):
- Mucosa
- Submucosa
- Muscularis propria
- Serosa
Margins
Each open end of a hollow organ is typically a margin where the surgeon has had to make an incision to separate the specimen from the organs that are in continuity with the specimen.
Thus, a segment of small bowel will have two cut ends (akin to chopping out a section of hosepipe from the reel as a whole). In tubular organs such as the small bowel, these are known as the
longitudinal margins.
By contrast, the bag hollow organs are more complex. The gallbladder has only one longitudinal margin, the cystic duct. Others, such as the uterus and bladder, possess only one main longitudinal margin (the junction with the vagina and the urethra respectively) but also have two narrow calibre input tubes (the fallopian tubes and ureters). Organs such as the bladder and uterus may be conceptualised as a letter Y with regard to their longitudinal margins.
After the longitudinal margins is the more thorny concept of the circumferential or radial margin and its distinction from a
surface.
Hollow organs do not simply dangle from their longitudinal margins within a body cavity. Instead, they have some attachment either to adjacent organs and/or the wall of the cavity. In order to remove the organ the surgeon must cut through these attachments.
Particularly in the case of attachments to the wall of the body cavity the term
pedicle may be adopted to refer to this attachment.
Blood vessels, lymphatic and nerves typically gain access to the organ via the pedicle and thus the pedicle provides not only support to hold the organ in place but is also a conduit for the neurovascular supply of the organ.
These attachments constitute the radial or circumferential margin. In the case of the small bowel this margin is formed by the apex of the mesentery. It occupies only a small portion of the perimeter of the specimen and may therefore be referred to by the term radial. By contrast, the rectum is entirely encased is mesorectal fat and the surgeon has to incise around the complete circumference of this fat to remove the rectum. Thus the term circumferential margin is employed.
|
|
|
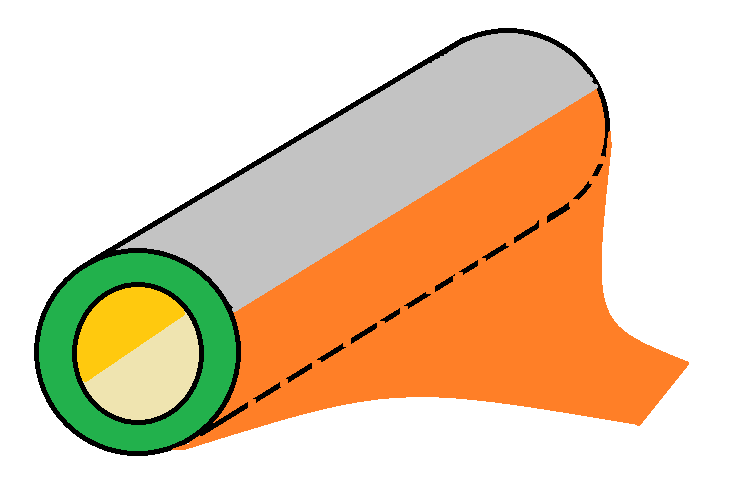
A simplified tubular hollow organ. The pedicle is shown in orange.
|
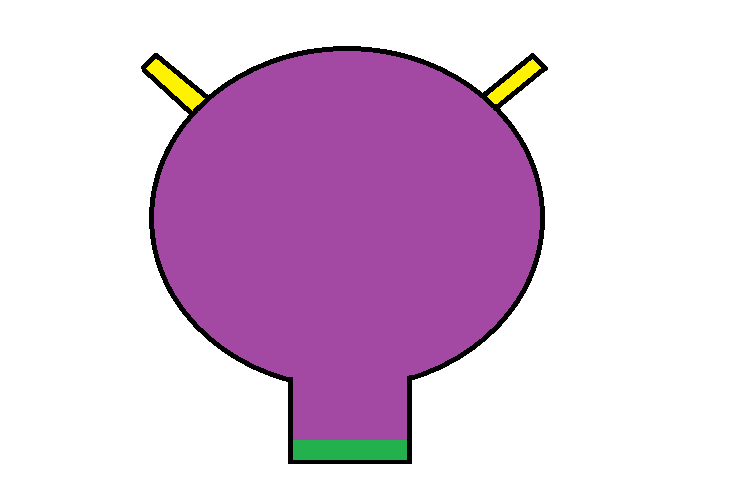
A simplified bag hollow organ. The main longitudinal margin is shown in green. The input tubes are in yellow.
|
|
|
|
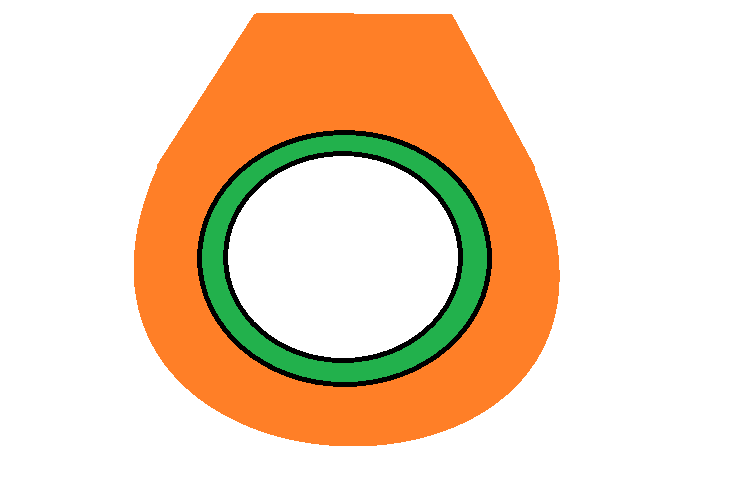
A hollow organ which is encased in a circumferential margin (orange). The pedicle comes to a plateau as it approaches the abdominal wall. An analogy with a sling is tempting.
|
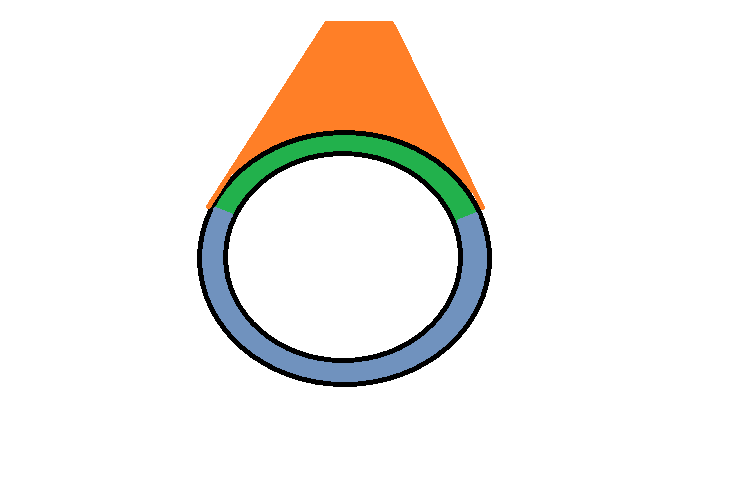
A hollow organ which has a radial margin. The pedicle is shown in orange. The part of the wall of the organ shown in blue is a surface. That in green is covered by the pedicle.
|
Staging
The staging of the primary tumour in the TNM system in hollow organs is generally determined by how far through the layers of the wall of the organ that tumour invades, whether it breaches the surface and whether it invades adjacent organs.
Different organs may have variations on this theme but the general principle holds. From this premise arises the requirement to take blocks of the tumour which can show this depth of invasion.
The lymph nodes of hollow organs tend to be submitted attached to the organ and determine the N stage of the TNM system. Additional lymph nodes may also be sent in separate pots. The attached lymph nodes are usually contained with a volume of fibrofatty tissue and this must be dissected in order to locate the lymph nodes.

|
|
|
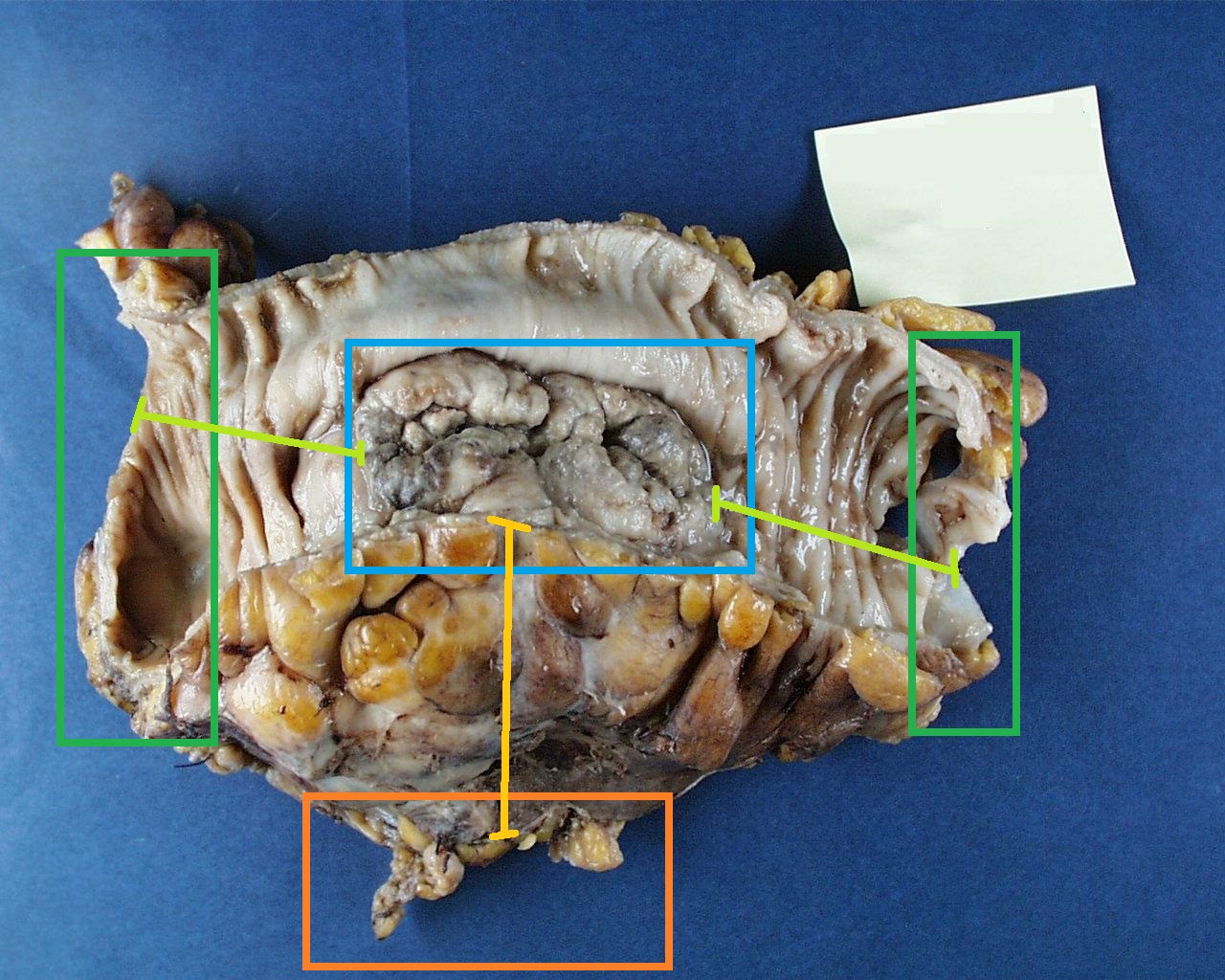
The short segment of colon has been opened longitudinally to disclose a relatively flat, irregular, ulcerated tumour in the middle of the specimen.
|
The same colon with blocks and margins indicated
Blue : tumour
Dark green : longitudinal margins
Light green : distance to longitudinal margins
Orange : radial (pedicle) margin
Orange-yellow : distance to the radial margin
|
Description
When describing a hollow organ a basic template can be used. Different organs will have different nuances but the general principles remain.
Tubular Hollow Organ
- Length
- Diameter or circumference (if asymmetrical, give two perpendicular diameters)
- Thickness of the wall
- Distance of the apex of the pedicle from the wall of the organ
- Description of the background mucosa and the serosal surface
- Length, width and thickness of the tumour
- Depth of invasion of the tumour through the layers of the wall
- Distance of the tumour from the longitudinal margins
- Distance of the tumour from the radial / circumferential margin
An example description of an oesophagectomy specimen is given below.
The specimen comprises a segment of oesophagus that measures 150mm in length by 25mm in circumference. The wall thickness is 10mm. No orientating markers are present to allow the proximal and distal ends to be distinguished.
The adventitial surface is unremarkable.
Located 60mm from one margin and and 70mm from the opposite longitudinal margin is an ulcerated tumour that occupies approximately half of the circumference. The tumour measures 20mm in length by 15cm in width and invades to a depth of 10mm. The tumour appears to invade through the muscularis propria into the adventitia and abuts the circumference of the specimen.
The oesophagus away from the tumour is unremarkable.
Bag Hollow Organs
- Three perpendicular diameters (may sometimes be referred to as height, width and depth or other anatomical designations)
- Thickness of the wall
- Lengths and diameters of the input tubes
- Thickness of any encasing soft tissue
- Description of the background mucosa and the serosal surface
- Length, width and thickness of the tumour
- Depth of invasion of the tumour through the layers of the wall
- Distance of the tumour from the longitudinal margins
- Distance of the tumour from the radial / circumferential margin
An example of a cystectomy report is given below.
The specimen comprises a cystectomy that measures 40mm in height by 30mm in transverse dimension and 30mm in anteroposterior dimension. The thickness of the wall is 5mm.
The attached right ureter measures 15mm long by 3mm in diameter. The attached left ureter is 20mm long and 3mm in diameter.
The external aspect of the specimen is unremarkable.
Situated on the posterior wall of the bladder within the trigone is an ulcerated, exophytic tumour that measures 22mm by 14mm and has a thickness of 8mm. The tumour appears to be confined to the wall of the bladder.
The tumour is 11mm from the urethral margin, 27mm from the right ureteric margin, 29mm from the left ureteric margin and 12mm from the circumferential margin.
The mucosa away from the tumour is unremarkable.
Block Taking
There are basic principles of sampling a hollow organ that will account for most blocks taken from most hollow organs.
All longitudinal margins should be sampled. This will usually be with an en face block of the entire margin but sometimes cruciate blocks will be required.
The blocks of the tumour must allow the type of tumour to be determined, its depth of invasion through the planes of the organ and its relationship to both the circumferential anatomical surface and the circumferential margin (if present). The blocks that are taken to accomplish this will usually suffice to evaluate other important parameters such as lymphatic invasion, vascular invasion, perineural invasion and immunohistochemical properties.
A block of the background normal tissue is useful to determine if any underlying disease that predisposed to the development of the tumour is present.