Contents
Introduction
General Clinical Aspects
Investigations
Introduction
Respiratory medicine is concerned primarily with diseases of the lungs but also encompasses disorders of the pleura and rarely may have to consider diseases of the chest wall and musculoskeletal system which impinge on the mechanics of breathing. The nomenclature of the specialty is unusual in that no name ending in -ology has ever been successfully appended.
General Clinical Aspects
Diseases of the lungs tend to produce a fairly limited number of symptoms, although the nuances of these symptoms (such as duration) and their combination allows quite reliable diagnosis.
Dyspnoea
Dyspnoea is shortness of breath. Any lung disease can cause dyspnoea but the symptom is not restricted to a pulmonary aetiology. Instead, various systems must be considered.
- Lungs
- Pleura
- Cardiovascular
- Head and neck
- Haematological (anaemia)
- Endocrine (hyperthyroidism)
- Musculoskeletal
- Neurological
Dyspnoea can arise when the arterial partial pressure of oxygen falls or the arterial partial pressure of carbon dioxide rises or blood pH drops. A sense of breathless may also be induced by circulating catecholamines.
Cough
Cough is another common symptom of lung disease. As with dyspnoea it is important not to overlook the possibility of an inhaled foreign body, especially in children.
A cough may be either productive, in which sputum is expelled by coughing, or non-productive. If a cough is productive it is important to ascertain the nature of the sputum, particularly its colour.
Coughing is a protective action that is intended to clear material from the airways. It may be stimulated by the presence of material, such as pus, in the airways but also by damage to the wall of the airways.
Haemoptysis
Haemoptysis is coughing up blood and implies damage to the mucosa of the airways. Although it can be a sinister symptom due to its occurrence in carcinoma, it may also be encountered in pneumonia, as well assorted other diseases.
Chest Pain
Chest pain is a major feature of surprisingly few lung diseases and is often due as much to damage to the pleura as the lungs themselves.
Hoarse Voice
A hoarse voice is potentially a worrying symptom in respiratory medicine, assuming that it cannot be safely attributed to laryngitis. The left recurrent laryngeal nerve detours through the mediastinum on its way to the larynx and can become damaged by mediastinal disease. The lung's main contribution to this phenomenon is bronchial carcinoma.
Associated Questions
As well as exploring the presenting complaint in the usual fashion there are several parameters which it is important to ascertain in the history of the presentng complaint for a respiratory problem.
- Smoking history
- History of asthma
- History of allergies / hay fever
- Family history of asthma or allergies
- Travel abroad
- Exposure to tuberculosis
- Occupation, including reference to chemical exposure
- Hobbies
- Pets (especially birds)
- Asbestos exposure
Various clinical signs can be elicited on the examination of the respiratory system. An overview of some of the more common and/or important features is given below.
Respiratory Rate
The normal respiratory rate for an adult is 12-16 breaths per minute. An increase above normal is referred to as tachypnoea.
As well as just counting the respiratory rate other observations can also be made, such as whether or not the patient appears to be distressed, is using their accessory muscles of respiration and whether or not they are able to talk in complete sentences.
Cyanosis
Cyanosis is a blue discolouration of the skin and/or mucous membranes. Cyanosis occurs when the blood contains at least 5g/dL of deoxygenated haemoglobin. It may be peripheral or central. Central cyanosis affects the lips and tongue and implies a defect in the oxygenation of the blood and therefore pulmonary or cardiac disease (or mechanical occlusion of the airways). Peripheral cyanosis occurs in the hands (and feet) and while it shares the causes of central cyanosis, it may also reflect a local problem in which there is reduced blood flow. Central cyanosis is generally the more serious symptom.
Trachea
The trachea should normally be positioned centrally in the neck. It remains in this position in most lung diseases but may deviate to one side if it is pushed by a mass lesion or is pulled by fibrosis.
Expansion
The expansion of the lungs is assessed by placing the hands on the chest in a specific fashion. The normal expansion of the lungs should be symmetrical. If one lung, or part of one lung, is not ventilated then the expansion will be reduced in that region.
Percussion
The lungs should be an air-filled organ and like any empty container should therefore make a resonant sound if tapped. Percussion of the chest is a technique for eliciting that sound. If the quantity of air in the percussed region of the thorax is reduced then the percussion note will sound dull rather than resonant. A hyperresonant percussion note can be encountered in a few situations.
Breath Sounds
By the time the stethoscope is actually placed onto the chest to listen to the lungs the examination of the respiratory system is almost finised. The normal pattern of the breath sounds is described as vesicular. Breath sounds may be either increased or decreased in intensity (if not normal); the altered sound in pneumonia is described as bronchial breathing, although this pattern is normal when heard over the upper airways.
Additional sounds may also be heard. Wheezes are high pitched noises which occur when the airways are narrowed. Crackles resemble two strips of velcro being pulled apart and are heard when the airways are stiff and/or difficult to open.
Examples of breath soulds may be heard at the following
link
Vocal Resonance
Vocal resonance is one of those aspects of the physical examination where the patient may wonder exactly what is happening because it involves the doctor auscultating the lungs while the patient says 'ninety-nine'. The theory behind this curious action is that if the airspaces of the lungs contain liquid they will transmit sound better and thus the patient's words will be heard more loudly than expected through the stethoscope. A variant of this test can be done by palpating instead of listening and is known as tactile vocal fremitus. The phrase 'ninety-nine' is chosen because of repeated 'n' sound.
Investigations
There are numerous investigations that may be called upon in the diagnosis of a respiratory problem but a few merit further elaboration at this juncture.
Peak Expiratory Flow Rate
The peak expiratory flow rate is the maximum flow of air that is achieved during a forcible expiratory effort. It can easily be measured at the bedside, in the outpatient clinic, at home or anywhere the patient cares to take the small, light handheld device.
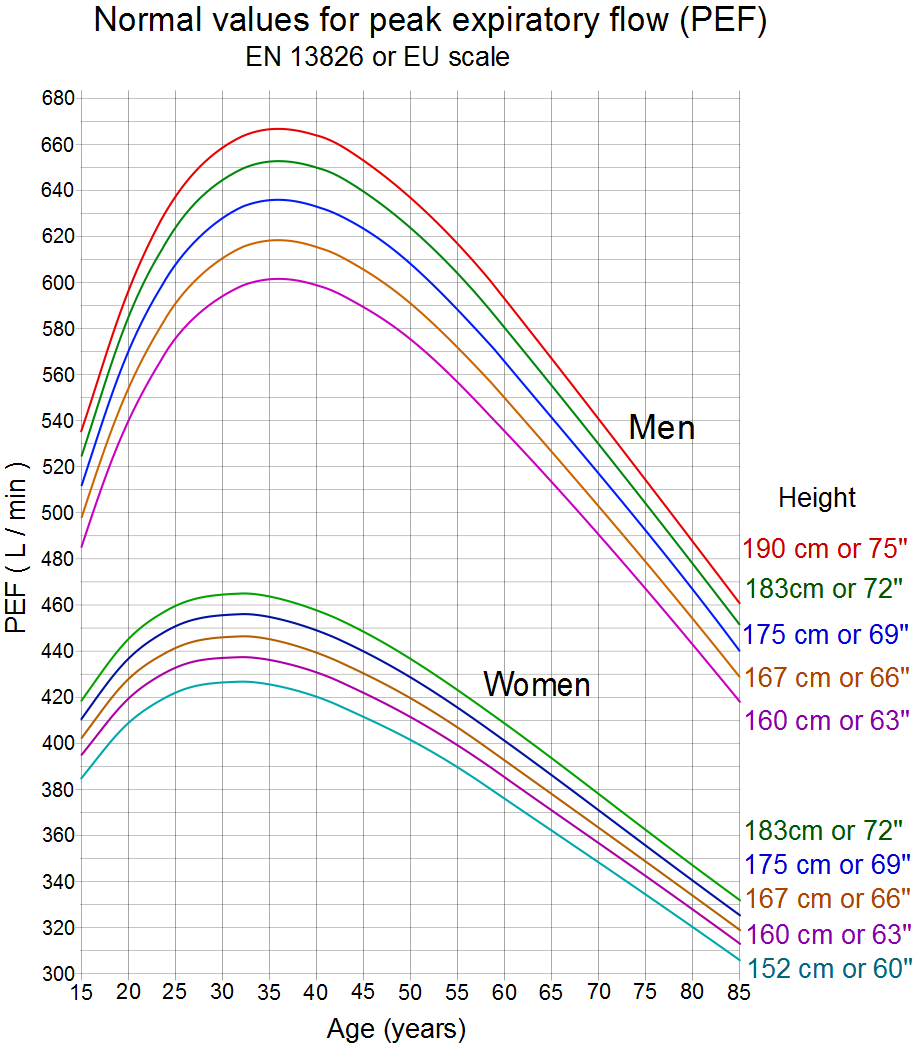
The normal range for the PEFR is very dependent upon age, sex and height.
The PEFR is very useful in the assessment of
asthma and
chronic obstructive pulmonary disease.
|

|
Graph of the ranges of peak expiratory flow rate
Image courtesy of Wikipedia
|
A peak expiratory flow meter
Image courtesy of Wikipedia
|
Lung Function Tests
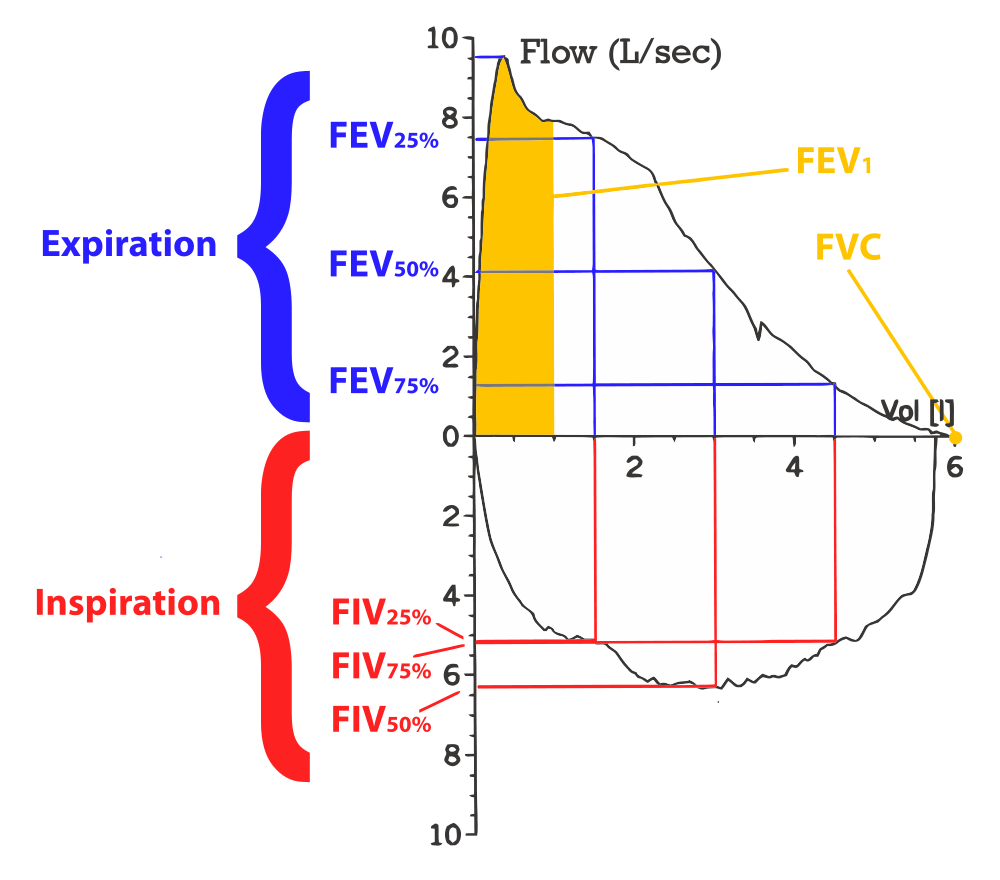
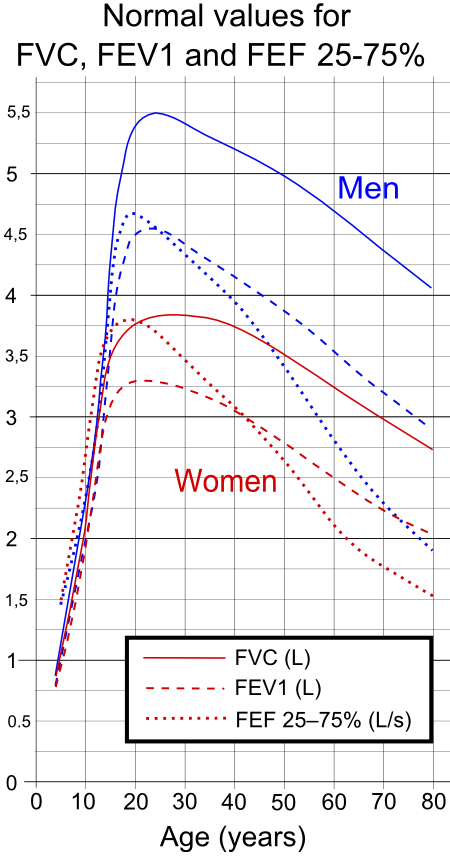
Lung function tests may sometimes be referred to as spirometry. They involve the measurement of various
functional lung volumes. The volumes are supplemented by assessment of the rates of air flow throughout the cycle of breathing in and breathing out. Different patterns of results can be obtained and may be useful in determing the type of lung disease.
Two main patterns of disease are described: obstructive and restrictive. In obstructive lung disease the FEV1/FVC ratio is decreased below 80% but the lung volumes may actually be increased. In restrictive lung disease the FEV1/FVC ratio is preserved but the lung volumes are reduced.
The lung volumes of spirometry allude to the space in the lungs that is available for air and not to the volumes of the lungs (tissue and air) themselves.
|
|
A flow volume loop
Image courtesy of Wikipedia
|
Graph of the ranges of FEV1 and related parameters
Image courtesy of Wikipedia
|
Lung function tests also include a measure of the diffusion capacity, which indicates how effeciently the lungs transfer oxygen into the blood and carbon dixoide out of the blood.
Arterial Blood Gases
Measurement of lung volumes can yield valuable information as to the function of the lungs but the fundamental test to determine whether or not the lungs are working properly is to measure the partial pressures of oxygen and carbon dioxide in the arterial blood.
Pulse oximetry is a simpler technique which uses reflected light to determine the percentage saturation of haemoglobin by oxygen but it does not give information regarding the partial pressure of carbon dioxide (or oxygen) or the blood pH. Furthermore, the
oxygen dissociation curve of haemoglobin means that the saturation may be quite high even though the partial pressure of oxygen is reduced. Therefore, if accurate knowledge of the gas transferring function of the lungs is required in an acute situation (the diffusion capacity requires special equipment and cannot be done at the bedside) an arterial blood gas sample must be obtained.
The radial artery is the usual site from which arterial blood gases are obtained. The femoral artery is the back up. The procedure can be more uncomfortable for the patient than taking a venous blood sample but the partial pressures and pH values found in a venous sample are confounded by tissue metabolism and so an arterial sample is necessary.
The normal range for the partial pressure of oxygen in an arterial blood gas sample depends upon the concentration of oxygen in the inspired air. Thus, an arterial blood gas result must state whether the patient is receiving oxygen and if so at what concentration.
The greater diffusing capacity of carbon dioxide over oxygen means that when the lungs start to fail, oxygen levels drop before carbon dioxide levels rise. In acute respiratory impairment a rising partial pressure of carbon dioxide is considered to be more serious than a low oxygen because it implies a greater degree of pulmonary impairment.
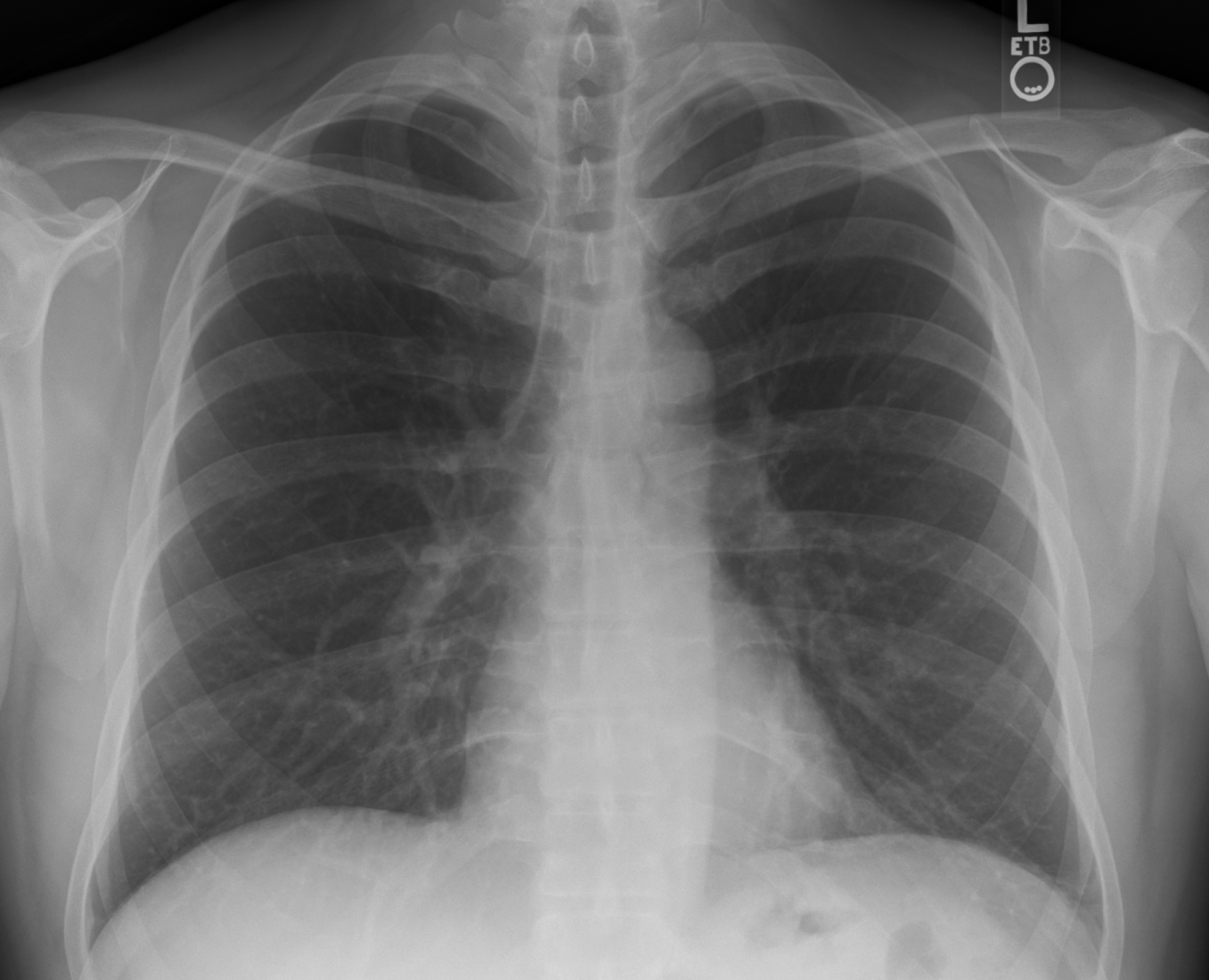
Chest X-Ray
The chest X-ray is one of the oldest forms of radiology. Despite lacking the sophistication of a CT or MRI scan it can neverthless yield a considerable degree of useful information. Furthermore it is more easily performed than a CT or MRI scan and can be undertaken at the ward using a portable machine.
The preferred method for taking a chest X-ray is to project the X-rays from behind the patient through to a plate / sensor on the anterior aspect of the chest. This is known as a PA chest X-ray. The alternative is to project the X-rays from front to back (an AP film). The PA is preferred because there is a lesser degree of magnification of the cardiac shadow and the procedure involves the patient abducting their arms which rotates the scapulas out of much of the field. The PA method is the one undertaken if the patient has their chest X-ray performed in the radiology department. The AP technique is adopted if a portable X-ray machine is used and reflects the fact that is easier to place the film / sensor behind the patient in their bed and project the X-rays from the front that it is to attempt a PA arrangement with a sick patient in bed on a ward.
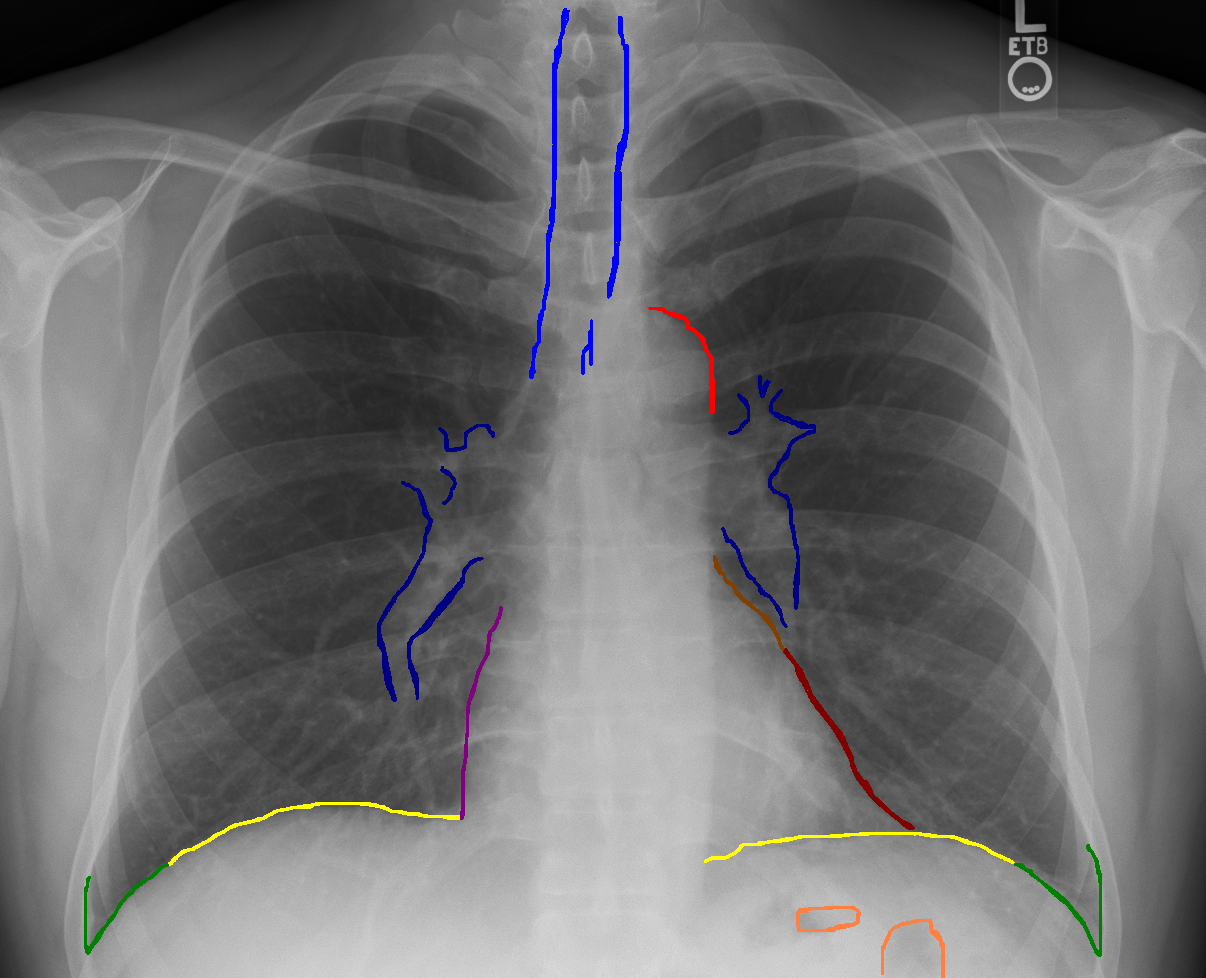
A chest X-ray demonstrates considerably more than just the lung fields. The outline of the heart is shown, as is the contour of the diaphragm and a small part of the abdomen immediately under the diaphgram. The trachea, aortic arch, clavicle and ribs are all displayed, as are the hilar of the lungs and the main pulmonary arteries.
|
|
A chest X-ray
Red - aortic arch
Brown - border of left atrium
Maroon - lower part of the left border of the heart
Purple - edge of the right atrium
Dark blue - pulmonary artery
Mid blue - trachea
Yellow - upper surface of the diaphragm
Green - costophrenic angle (including lateral part of the diaphragm)
Orange - gas in the GI tract
|
The same chest X-ray without labelling
|